What is the best diet for irritable bowel syndrome – What’s the best diet for irritable bowel syndrome? It’s a question that plagues millions, as the condition impacts digestion and quality of life. Understanding IBS, its causes, and its relationship with diet is crucial for effective management. This article explores various dietary approaches, from general recommendations to specific diets like FODMAP and low-residue, aiming to provide valuable insights for individuals seeking relief from IBS symptoms.
While there’s no one-size-fits-all solution, dietary modifications play a significant role in alleviating IBS discomfort. We’ll delve into the impact of food triggers, sensitivities, and intolerances, shedding light on how specific foods can exacerbate symptoms. We’ll also examine the importance of hydration, fiber intake, and the potential benefits of stress management, exercise, and sleep hygiene in managing IBS effectively.
Understanding Irritable Bowel Syndrome (IBS)
Irritable bowel syndrome (IBS) is a common disorder that affects the large intestine. It causes a variety of symptoms, including abdominal pain, bloating, gas, diarrhea, and constipation. While IBS is not life-threatening, it can significantly impact a person’s quality of life.
Symptoms of IBS
IBS symptoms can vary widely from person to person. Some people experience mild symptoms, while others have severe symptoms that significantly disrupt their daily lives. The most common symptoms include:
- Abdominal pain or discomfort
- Bloating and gas
- Diarrhea
- Constipation
- Changes in bowel habits
- Mucus in the stool
- Feeling of incomplete bowel movements
- Urgency to have a bowel movement
Types of IBS
There are different types of IBS, classified based on the predominant symptoms:
- IBS with diarrhea (IBS-D): This type is characterized by frequent loose stools and a feeling of urgency to have a bowel movement.
- IBS with constipation (IBS-C): This type is characterized by infrequent, hard stools and difficulty passing them.
- IBS with mixed bowel habits (IBS-M): This type is characterized by alternating periods of diarrhea and constipation.
- Unspecified IBS: This type is used when the predominant symptom pattern doesn’t fit into the other categories.
Causes and Risk Factors of IBS
The exact cause of IBS is unknown, but it is believed to be a combination of factors, including:
- Changes in gut bacteria: The balance of bacteria in the gut, known as the microbiome, can play a role in IBS development.
- Abnormalities in the gut’s nervous system: The gut has its own nervous system, known as the enteric nervous system, which can be affected in IBS.
- Inflammation in the gut: While IBS is not an inflammatory bowel disease, some inflammation in the gut may occur.
- Genetic predisposition: IBS may be more common in people with a family history of the condition.
- Psychological factors: Stress, anxiety, and depression can worsen IBS symptoms.
- Food sensitivities: Certain foods, such as dairy, gluten, and caffeine, can trigger IBS symptoms in some people.
- Previous gastrointestinal infections: A history of infections in the gut can increase the risk of developing IBS.
The Role of Diet in IBS Management
Diet plays a crucial role in managing Irritable Bowel Syndrome (IBS) symptoms. Understanding the impact of food on IBS and identifying potential triggers can significantly improve your quality of life.
Common Food Triggers for IBS
Food triggers vary from person to person, but certain foods are known to commonly exacerbate IBS symptoms. These triggers can irritate the digestive system, leading to bloating, gas, diarrhea, or constipation.
- High-fiber foods: While fiber is generally beneficial, excessive intake can cause discomfort for some individuals with IBS. Examples include legumes (beans, lentils), cruciferous vegetables (broccoli, cauliflower), and whole grains.
- Fatty foods: Foods high in fat can slow down digestion and increase the risk of bloating and diarrhea. Examples include fried foods, processed meats, and fatty sauces.
- Dairy products: Lactose intolerance, a common condition, can trigger IBS symptoms. Symptoms include bloating, gas, and diarrhea after consuming dairy products like milk, cheese, and yogurt.
- Carbonated beverages: Carbonation can contribute to gas and bloating, especially in individuals with IBS.
- Artificial sweeteners: Some artificial sweeteners, such as sorbitol and mannitol, can have a laxative effect and may worsen IBS symptoms.
- Spicy foods: Spicy foods can irritate the digestive tract and lead to discomfort, particularly in individuals with IBS.
- Alcohol: Alcohol can worsen IBS symptoms by irritating the digestive system and potentially causing dehydration.
- Caffeine: Caffeine can have a stimulating effect on the digestive system and may increase the frequency of bowel movements.
Food Sensitivities and Intolerances
Food sensitivities and intolerances can also contribute to IBS symptoms. These are different from allergies, which involve an immune response.
- Food sensitivity: This involves a delayed reaction to certain foods, often causing symptoms like bloating, gas, and digestive discomfort hours or days after consumption. Common examples include gluten, dairy, and histamine.
- Food intolerance: This involves an inability to digest certain foods properly, often due to a lack of specific enzymes. Examples include lactose intolerance, which involves a deficiency in the enzyme lactase needed to digest lactose, the sugar found in dairy products.
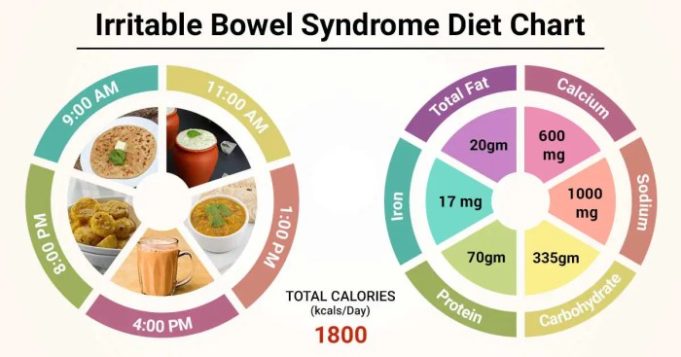
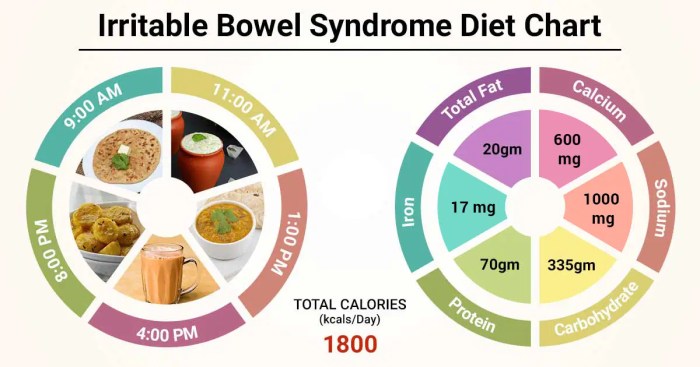
General Dietary Recommendations for IBS
The goal of dietary management for IBS is to identify and eliminate trigger foods that worsen symptoms while promoting a balanced and healthy diet. This involves understanding individual food sensitivities, adopting a personalized approach, and gradually introducing new foods to assess their impact.
Recommended Foods for Individuals with IBS
A balanced diet for IBS typically includes a variety of nutrient-rich foods that are gentle on the digestive system. Here are some recommended food groups:
- Fruits: Apples, bananas, berries, melons, pears, and cooked fruits like applesauce.
- Vegetables: Cooked leafy greens, carrots, sweet potatoes, zucchini, and asparagus.
- Grains: Gluten-free options like rice, quinoa, oats, and corn.
- Proteins: Lean meats, poultry, fish, eggs, tofu, and beans (in moderation).
- Dairy: Lactose-free milk, yogurt, and cheese.
Importance of Hydration and Fiber Intake for IBS
Adequate hydration is crucial for maintaining regular bowel movements and preventing constipation, a common symptom of IBS. Aim for 8 glasses of water daily, along with other hydrating beverages like herbal teas and clear broth.
Fiber plays a vital role in digestive health, but its intake should be carefully managed in individuals with IBS. Soluble fiber, found in oats, beans, and fruits, absorbs water and forms a gel-like substance that can help regulate bowel movements. Insoluble fiber, found in whole grains and vegetables, adds bulk to stools and promotes regularity.
It is important to note that excessive fiber intake can exacerbate IBS symptoms, especially in individuals with diarrhea-predominant IBS. Start with small amounts of fiber and gradually increase intake as tolerated.
Specific Diets for IBS
There are several specific diets that have been proposed for managing IBS symptoms. These diets aim to target specific food components that may trigger IBS symptoms in some individuals. Let’s delve into three popular diets: the FODMAP diet, the low-residue diet, and the gluten-free diet.
The FODMAP Diet
The FODMAP diet is a popular dietary approach for managing IBS symptoms. FODMAP stands for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols. These are short-chain carbohydrates that are poorly absorbed in the small intestine and can be fermented by bacteria in the large intestine, leading to gas, bloating, and other IBS symptoms.
The FODMAP diet involves a two-phase process:
- Phase 1: Elimination Phase: This phase involves eliminating high-FODMAP foods for 2-6 weeks. This helps identify which FODMAPs are triggering symptoms for an individual.
- Phase 2: Reintroduction Phase: Once symptoms have improved, individuals gradually reintroduce high-FODMAP foods one at a time, monitoring their response to identify their individual FODMAP tolerance levels.
The FODMAP diet has been shown to be effective in reducing IBS symptoms in many individuals. A 2015 study published in the journal “The American Journal of Gastroenterology” found that 75% of individuals with IBS experienced a significant improvement in their symptoms after following the FODMAP diet.
However, the FODMAP diet has some limitations. It can be challenging to follow long-term due to the restrictions on many common foods. Additionally, it requires close monitoring of symptoms and may require the guidance of a registered dietitian or other healthcare professional.
“The FODMAP diet can be a valuable tool for managing IBS symptoms, but it’s essential to work with a healthcare professional to ensure proper implementation and avoid potential nutritional deficiencies.”
The Low-Residue Diet
The low-residue diet is a dietary approach that restricts foods that are high in fiber and other indigestible substances. This diet is often recommended for individuals with IBS who experience diarrhea or who have had recent bowel surgery.
The low-residue diet emphasizes foods that are easily digested and leave minimal residue in the colon. This includes:
- Low-fiber fruits and vegetables: such as bananas, cooked apples, and peeled carrots.
- White rice and white bread: These are lower in fiber than whole-grain options.
- Lean meats, poultry, and fish: These are good sources of protein and are low in fiber.
- Cooked vegetables: These are easier to digest than raw vegetables.
The low-residue diet can be effective in reducing diarrhea and other IBS symptoms, but it is often considered a short-term solution. Long-term adherence to this diet can lead to nutrient deficiencies, and it may not be suitable for everyone with IBS.
“The low-residue diet can provide temporary relief from IBS symptoms, but it’s crucial to consult with a healthcare professional to ensure adequate nutrition and address potential long-term consequences.”
The Gluten-Free Diet
The gluten-free diet eliminates gluten, a protein found in wheat, barley, and rye. While gluten sensitivity is a recognized condition, it is not a common cause of IBS. However, some individuals with IBS may experience symptom relief on a gluten-free diet, even if they do not have celiac disease or gluten sensitivity.
“While the gluten-free diet may help some individuals with IBS, it’s not a standard treatment and should only be considered after ruling out celiac disease and other potential causes of IBS symptoms.”
The gluten-free diet can be challenging to follow long-term due to the restrictions on many common foods. It’s important to ensure that gluten-free foods are adequately fortified with essential nutrients, and it’s recommended to consult with a registered dietitian to ensure a balanced diet.
“A gluten-free diet may offer some relief for certain individuals with IBS, but it’s essential to ensure proper nutrition and consult with a healthcare professional to determine if it’s the right approach.”
Lifestyle Modifications for IBS
Living with IBS often involves making lifestyle changes to manage symptoms. These modifications can significantly improve your quality of life and help you control your IBS.
Stress Management
Stress is a significant trigger for IBS symptoms. When you’re stressed, your body releases hormones that can affect your digestive system, leading to increased pain, bloating, and diarrhea or constipation.
- Practice relaxation techniques: Techniques like deep breathing exercises, meditation, and yoga can help calm your mind and body, reducing stress levels.
- Engage in activities you enjoy: Hobbies, spending time with loved ones, and engaging in activities that bring you joy can help reduce stress.
- Seek professional help: If stress is a significant issue in your life, consider seeking professional help from a therapist or counselor.
Regular Exercise
Regular physical activity can benefit your overall health and help manage IBS symptoms. Exercise helps regulate bowel movements, reduces stress, and improves mood.
- Aim for at least 30 minutes of moderate-intensity exercise: This could include brisk walking, swimming, cycling, or dancing.
- Start slowly and gradually increase the intensity and duration: Listen to your body and avoid overexertion, especially if you’re new to exercise.
- Find an activity you enjoy: This will make it more likely that you’ll stick with it.
Sleep Hygiene
Getting enough sleep is crucial for managing IBS. Lack of sleep can worsen IBS symptoms, including pain, bloating, and diarrhea.
- Establish a regular sleep schedule: Go to bed and wake up around the same time each day, even on weekends.
- Create a relaxing bedtime routine: This could include taking a warm bath, reading a book, or listening to calming music.
- Make sure your bedroom is dark, quiet, and cool: These conditions promote better sleep.
- Avoid caffeine and alcohol before bed: These substances can interfere with sleep.
Identifying and Avoiding Food Triggers
Food triggers are specific foods that worsen IBS symptoms. Identifying and avoiding these triggers is essential for managing your condition.
- Keep a food diary: Record what you eat and drink, along with any symptoms you experience. This can help you identify potential triggers.
- Eliminate suspected triggers one at a time: Avoid a specific food for a few weeks to see if your symptoms improve.
- Reintroduce foods gradually: Once you’ve eliminated a trigger, reintroduce it slowly to see if it causes symptoms.
Seeking Professional Guidance
While this guide provides valuable information about IBS and dietary approaches, it’s crucial to remember that it’s not a substitute for professional medical advice. Consulting a healthcare professional is essential for a proper diagnosis and personalized management plan.
The Importance of Consulting a Healthcare Professional
A healthcare professional can accurately diagnose IBS, rule out other underlying medical conditions, and provide tailored recommendations based on your individual needs. They can help you understand the causes of your symptoms, explore various treatment options, and address any concerns you may have.
The Role of a Registered Dietitian in IBS Management
A registered dietitian (RD) is a qualified nutrition expert who can help you create a personalized dietary plan to manage your IBS symptoms. They can provide guidance on:
- Identifying trigger foods that exacerbate your symptoms.
- Developing an individualized meal plan that meets your nutritional needs and helps manage IBS.
- Educating you about dietary strategies to improve digestion and reduce discomfort.
Available Treatments and Medications for IBS, What is the best diet for irritable bowel syndrome
In addition to dietary modifications, several treatments and medications can help manage IBS symptoms. These include:
- Anti-diarrheal medications: These medications help to slow down bowel movements and reduce diarrhea. Examples include loperamide (Imodium) and bismuth subsalicylate (Pepto-Bismol).
- Antispasmodic medications: These medications relax the muscles in the digestive tract, reducing cramping and pain. Examples include hyoscyamine and dicyclomine.
- Antidepressants: Some antidepressants, particularly tricyclic antidepressants, can be effective in managing IBS symptoms, even if you don’t have depression. They work by regulating the nervous system and reducing pain signals.
- Probiotics: These are live bacteria that can help restore the balance of gut bacteria. Some studies suggest that probiotics may be beneficial for IBS, particularly for diarrhea-predominant IBS.
- Fiber supplements: While high-fiber diets can trigger IBS symptoms in some people, soluble fiber supplements like psyllium husk can help regulate bowel movements and reduce constipation.
Concluding Remarks
Ultimately, finding the best diet for IBS involves a personalized approach. Working with a healthcare professional, particularly a registered dietitian, can provide tailored guidance and support. By understanding the intricacies of IBS and implementing a balanced dietary strategy, individuals can empower themselves to manage symptoms and improve their overall well-being.
FAQs: What Is The Best Diet For Irritable Bowel Syndrome
Can I cure IBS with diet alone?
While diet can significantly improve symptoms, it’s not a cure for IBS. Managing stress, exercise, and sometimes medication may also be necessary.
What are some common food triggers for IBS?
Common triggers include dairy, gluten, beans, onions, garlic, and high-fiber foods. However, individual triggers can vary.
How long does it take to see results from a dietary change for IBS?
It can take several weeks to a few months to notice significant improvement in symptoms after dietary modifications.
Is it safe to try a specific diet for IBS without consulting a doctor?
It’s always best to consult a healthcare professional before making significant dietary changes, especially if you have underlying health conditions.
Finding the best diet for irritable bowel syndrome (IBS) often involves trial and error. A common element in many successful IBS diets is the reduction of sugar intake, which can exacerbate symptoms. If you’re looking to cut down on sugar, a great resource is how to eliminate sugar from your diet.
By making these adjustments, you may find relief from IBS symptoms and improve your overall gut health.
Finding the best diet for irritable bowel syndrome (IBS) can be a bit of a journey. It often involves experimenting with different foods and identifying triggers. A key aspect is to understand the best way to diet in general, which includes gradual changes, mindful eating, and listening to your body.
This approach can help you pinpoint what works best for your individual IBS symptoms and ultimately improve your overall gut health.
Finding the best diet for irritable bowel syndrome (IBS) can be a journey of trial and error. Some people find relief with a low-FODMAP diet, while others benefit from a gluten-free approach. If you’re looking for more information on specific dietary approaches, you might want to check out if diet , which provides insights on various dietary plans and their potential impact on IBS.
Ultimately, the best diet for IBS is the one that works best for you, so it’s important to experiment and find what helps manage your symptoms.