What diet for diverticulitis? It’s a question many people with this common digestive condition ask. Diverticulitis, characterized by inflammation or infection in small pouches that form in the colon, can be a painful and disruptive experience. While there’s no single cure, understanding the role of diet in managing symptoms is crucial. This guide explores the basics of diverticulitis, delves into the importance of diet, and provides practical tips for navigating this condition.
By understanding the causes and potential complications, we can better grasp the importance of dietary modifications in preventing flare-ups and promoting overall digestive health. From high-fiber diets to low-residue options, we’ll discuss various dietary approaches and their potential benefits.
Understanding Diverticulitis
Diverticulitis is a common condition that affects the digestive system. It occurs when small pouches, called diverticula, form in the lining of the colon. These pouches can become inflamed or infected, leading to pain, fever, and other symptoms.
Causes of Diverticulitis
Diverticula are common, and most people who have them never experience any problems. However, in some cases, these pouches can become inflamed or infected, leading to diverticulitis. The exact cause of diverticulitis is unknown, but it is thought to be related to a combination of factors, including:
- Low-fiber diet: A diet low in fiber can lead to constipation and increased pressure in the colon, which can contribute to the formation of diverticula.
- Aging: The risk of diverticulitis increases with age.
- Genetics: Some people may be genetically predisposed to developing diverticulitis.
- Obesity: Obesity is associated with an increased risk of diverticulitis.
- Smoking: Smoking can also increase the risk of developing diverticulitis.
Symptoms of Diverticulitis
The symptoms of diverticulitis can vary depending on the severity of the condition. Some people may experience mild symptoms, while others may have severe symptoms that require hospitalization. Common symptoms of diverticulitis include:
- Abdominal pain: Pain is usually located in the lower left abdomen, but it can also occur in other areas of the abdomen.
- Fever: A fever is a common symptom of diverticulitis, especially if the condition is severe.
- Nausea and vomiting: These symptoms are common in people with diverticulitis.
- Diarrhea or constipation: Changes in bowel habits are common in people with diverticulitis.
- Blood in the stool: Blood in the stool is a sign of a more serious complication of diverticulitis.
Stages of Diverticulitis
Diverticulitis is typically classified into four stages:
- Stage 1: This stage is characterized by mild inflammation of the diverticula. Symptoms may be mild or absent.
- Stage 2: This stage is characterized by more severe inflammation of the diverticula. Symptoms may include abdominal pain, fever, and nausea.
- Stage 3: This stage is characterized by an abscess, which is a collection of pus that forms near the inflamed diverticula. Symptoms may include severe abdominal pain, fever, and chills.
- Stage 4: This stage is characterized by a perforation, which is a hole in the colon wall. Symptoms may include severe abdominal pain, fever, and shock.
Complications of Diverticulitis
Diverticulitis can lead to a number of complications, including:
- Abscess: An abscess is a collection of pus that forms near the inflamed diverticula.
- Perforation: A perforation is a hole in the colon wall. This can lead to peritonitis, which is a serious infection of the abdominal cavity.
- Fistula: A fistula is an abnormal connection between the colon and another organ, such as the bladder or small intestine.
- Bleeding: Bleeding from the diverticula can occur, and it can be a serious complication.
- Obstruction: Inflammation and scarring from diverticulitis can lead to an obstruction of the colon.
The Role of Diet in Diverticulitis Management
Diet plays a crucial role in managing diverticulitis, both in preventing flare-ups and aiding recovery. While the exact cause of diverticulitis is unknown, it’s believed that a low-fiber diet and a lack of physical activity contribute to its development. Therefore, adopting a balanced dietary approach is essential for individuals with diverticulitis.
Fiber Intake and Its Importance
Fiber is an essential component of a healthy diet, particularly for managing diverticulitis. It helps regulate bowel movements, promoting regular stool passage and reducing pressure within the colon. This, in turn, can help prevent the formation of pouches (diverticula) in the colon wall and reduce the risk of inflammation.
High-Fiber Foods
Here are some examples of high-fiber foods that can be incorporated into a diverticulitis-friendly diet:
- Fruits: Apples, pears, berries, oranges, bananas
- Vegetables: Broccoli, Brussels sprouts, carrots, peas, spinach
- Whole grains: Brown rice, quinoa, oats, whole-wheat bread
- Legumes: Beans, lentils, chickpeas
- Nuts and seeds: Almonds, walnuts, flax seeds, chia seeds
Low-Residue Diet During Acute Flare-Ups, What diet for diverticulitis
During an acute diverticulitis flare-up, a low-residue diet is recommended. This diet focuses on reducing the amount of fiber and undigestible matter in the digestive tract, thereby minimizing irritation and inflammation.
Foods to Include
- White rice
- White bread
- Cooked vegetables without skins (e.g., peeled potatoes, carrots, squash)
- Lean meats
- Cooked fish
- Eggs
- Plain yogurt
Foods to Avoid
- High-fiber foods
- Raw fruits and vegetables
- Nuts and seeds
- Whole grains
- Spicy foods
- Fatty foods
- Alcohol
- Caffeine
Specific Diet Plans for Diverticulitis
A diverticulitis-friendly diet focuses on easing digestive discomfort and promoting healing. It involves consuming foods that are easily digested and avoiding those that can irritate the digestive tract. While there’s no one-size-fits-all approach, several diet plans can help manage diverticulitis symptoms.
Sample Meal Plan for a Typical Day
A typical day on a diverticulitis-friendly diet might look like this:
Breakfast: Oatmeal with berries and nuts, a smoothie with yogurt, fruit, and spinach, or scrambled eggs with whole-wheat toast.
Lunch: A salad with grilled chicken or fish, lentil soup, or a whole-wheat sandwich with lean protein and vegetables.
Dinner: Baked salmon with roasted vegetables, chicken stir-fry with brown rice, or vegetarian chili.
Snacks: Fruits, vegetables, yogurt, or nuts.
Foods to Include and Avoid
This table Artikels foods to include and avoid in a diverticulitis diet:
| Include | Avoid |
|---|---|
| High-fiber fruits and vegetables (berries, apples, pears, broccoli, spinach, carrots) | Low-fiber fruits and vegetables (bananas, grapes, white potatoes, corn) |
| Lean protein (chicken, fish, beans, lentils) | Red meat, processed meats |
| Whole grains (brown rice, quinoa, oats) | Refined grains (white bread, white rice) |
| Healthy fats (olive oil, avocado) | Saturated and trans fats |
| Plenty of water | Sugary drinks, alcohol |
Dietary Approaches for Diverticulitis
The BRAT Diet
The BRAT diet (Bananas, Rice, Applesauce, Toast) is a bland diet often recommended for mild cases of diverticulitis. It aims to rest the digestive system by providing easily digestible foods. However, it’s not a long-term solution as it lacks essential nutrients.
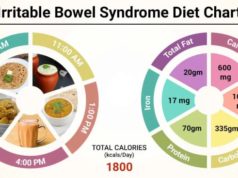
The Low-FODMAP Diet
The low-FODMAP diet focuses on limiting fermentable carbohydrates (FODMAPs) that can trigger digestive symptoms. It’s often used for irritable bowel syndrome (IBS), but it can also be helpful for diverticulitis. The low-FODMAP diet involves eliminating foods high in FODMAPs, such as dairy, wheat, garlic, onions, and certain fruits.
While both the BRAT and low-FODMAP diets can provide temporary relief, they are not intended for long-term use. It’s essential to consult with a healthcare professional to determine the best dietary approach for your individual needs.
Additional Considerations for Diet and Diverticulitis
While adhering to a low-fiber diet during an acute diverticulitis flare-up is crucial, it’s equally important to consider other factors that can influence your recovery and prevent future episodes.
Hydration
Staying adequately hydrated is vital for managing diverticulitis. Water helps soften stool, making it easier to pass and reducing strain on the digestive system. Aim for at least 8 glasses of water per day, especially during a flare-up. Other hydrating options include clear broth, herbal teas, and diluted fruit juices.
Food Sensitivities and Intolerances
Certain foods, even those typically considered low-fiber, can trigger diverticulitis symptoms in some individuals. Common culprits include:
- Dairy products: Lactose intolerance can cause bloating, gas, and diarrhea, exacerbating diverticulitis symptoms.
- Gluten: Some people with diverticulitis experience worsened symptoms when consuming gluten, a protein found in wheat, barley, and rye.
- Spicy foods: Spicy foods can irritate the digestive tract, potentially aggravating diverticulitis.
- Alcohol: Alcohol can irritate the stomach lining and worsen inflammation.
- Caffeine: Caffeine can stimulate bowel movements, which may be problematic during a flare-up.
If you suspect a food sensitivity, consult with your doctor or a registered dietitian to identify and eliminate potential triggers.
Preventing Future Flare-Ups
Dietary modifications play a crucial role in preventing future diverticulitis episodes. Here are some tips:
- Gradually increase fiber intake: After a flare-up, gradually reintroduce fiber-rich foods into your diet, starting with low-fiber options and increasing gradually. This allows your digestive system to adjust and prevents overwhelming it.
- Choose soluble fiber: Soluble fiber dissolves in water and forms a gel-like substance, which can help regulate bowel movements and prevent constipation. Good sources of soluble fiber include oats, beans, lentils, and flaxseeds.
- Limit processed foods: Processed foods often contain high amounts of sugar, unhealthy fats, and artificial ingredients that can irritate the digestive system and contribute to inflammation.
- Eat regular meals: Skipping meals can lead to overeating and digestive distress. Regular meal times help maintain a consistent blood sugar level and support healthy digestion.
- Stay active: Regular physical activity promotes healthy digestion and helps prevent constipation, a risk factor for diverticulitis.
Consulting with Healthcare Professionals: What Diet For Diverticulitis
While the information provided in this guide can be helpful, it is crucial to remember that every individual is different. Diverticulitis is a complex condition, and dietary recommendations can vary depending on the severity of your symptoms, underlying health conditions, and individual needs.
Therefore, it is highly recommended to consult with a healthcare professional, such as a doctor or a registered dietitian, for personalized dietary guidance.
Benefits of Consulting a Healthcare Professional
Collaborating with a healthcare professional offers numerous benefits when managing diverticulitis through diet.
- Personalized Diet Plan: A healthcare professional can assess your individual needs and create a tailored diet plan that addresses your specific symptoms and medical history.
- Safe and Effective Recommendations: They can provide evidence-based recommendations that are safe and effective for your condition, ensuring you avoid potentially harmful dietary choices.
- Address Underlying Health Conditions: If you have other health conditions, such as diabetes or heart disease, a healthcare professional can help you create a diet plan that accommodates both your diverticulitis and other medical needs.
- Monitor Progress and Adjust Diet: They can monitor your progress and adjust your diet plan as needed, ensuring it remains effective and helps you manage your symptoms effectively.
Resources and Support Groups
If you are struggling with diverticulitis, know that you are not alone. Numerous resources and support groups can provide valuable information, emotional support, and a sense of community.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): This organization offers comprehensive information about diverticulitis, including its causes, symptoms, treatment options, and dietary recommendations. You can access their website and resources at [website address].
- Crohn’s & Colitis Foundation: Although focused on inflammatory bowel diseases, this foundation provides helpful information and support resources for individuals with diverticulitis, as the conditions share similarities in terms of digestive health.
- Local Support Groups: Many communities have local support groups for individuals with diverticulitis. These groups can offer a platform to connect with others who understand your condition and share experiences, coping strategies, and support.
Remember, seeking professional guidance is essential for managing diverticulitis effectively. A personalized diet plan, coupled with support from healthcare professionals and community resources, can significantly improve your well-being and quality of life.
Last Recap
Living with diverticulitis doesn’t have to be a constant battle. By making informed dietary choices and working closely with your healthcare provider, you can effectively manage symptoms and improve your quality of life. Remember, individual needs vary, so it’s essential to tailor your diet to your specific circumstances and consult with a registered dietitian for personalized guidance. By embracing a balanced and informed approach, you can navigate diverticulitis with greater confidence and ease.
Question Bank
Can I eat fruit if I have diverticulitis?
Yes, most fruits are beneficial for diverticulitis, but it’s best to choose soft, cooked, or peeled options. Avoid raw fruits with seeds or skins, as they can be difficult to digest.
What about alcohol and diverticulitis?
It’s generally recommended to limit or avoid alcohol, as it can irritate the digestive system and worsen symptoms.
Is there a specific type of fiber that’s better for diverticulitis?
Soluble fiber, found in foods like oats, beans, and lentils, is generally easier to digest and may be more beneficial for diverticulitis.
Can I exercise with diverticulitis?
Regular exercise is generally encouraged, but it’s important to listen to your body and avoid strenuous activities during flare-ups.
When it comes to diverticulitis, a high-fiber diet is often recommended. This helps to bulk up stools and make them easier to pass, reducing pressure on the diverticula. Speaking of diets, you might be wondering if is a raw diet good for dogs , and while it can be beneficial for some, it’s important to consult with a veterinarian to ensure it’s appropriate for your pet.
Back to diverticulitis, remember to talk to your doctor about the best diet plan for your specific needs.
A diet for diverticulitis focuses on high-fiber foods to help regulate digestion and prevent flare-ups. This can be challenging when trying to lose weight, as many popular weight-loss diets are low in fiber. However, there are ways to incorporate fiber-rich foods into different types of diets to lose weight, such as the Mediterranean diet or the DASH diet.
Learn more about various types of diets to lose weight and find one that fits your needs and diverticulitis management plan.
A diet for diverticulitis focuses on easing inflammation and promoting healthy digestion. This often involves consuming plenty of fiber, found in fruits, vegetables, and whole grains. To find out more about how to approach a healthy diet in general, check out this guide on the best way to diet.
Understanding the principles of healthy eating can help you create a sustainable dietary plan that supports your overall health and well-being, including managing diverticulitis.