Best diet to reduce cholesterol, a topic that concerns many, is not just about restricting food. It’s about understanding the different types of cholesterol, their impact on your health, and how to make smart dietary choices. Cholesterol, a waxy substance found in your blood, plays a crucial role in building healthy cells, but high levels can lead to serious health problems. This comprehensive guide will explore the science behind cholesterol, effective dietary strategies, and lifestyle modifications that can help you lower your cholesterol naturally and improve your overall well-being.
This guide will delve into the specifics of different diets like the Mediterranean and DASH, highlighting their unique benefits for cholesterol management. We’ll also explore the importance of regular physical activity, stress management, and weight control in maintaining healthy cholesterol levels. Finally, we’ll discuss the role of supplements and medications in addressing high cholesterol, providing information on their effectiveness and potential side effects.
Understanding Cholesterol: Best Diet To Reduce Cholesterol
Cholesterol is a waxy, fat-like substance found in all cells of the body. It is essential for building healthy cell membranes, producing hormones, and making vitamin D. However, high levels of cholesterol can lead to health problems.
Types of Cholesterol
Cholesterol exists in two main forms: low-density lipoprotein (LDL) and high-density lipoprotein (HDL).
- LDL cholesterol, often referred to as “bad” cholesterol, can build up in the arteries, forming plaque that restricts blood flow. This can increase the risk of heart disease and stroke.
- HDL cholesterol, often referred to as “good” cholesterol, helps remove LDL cholesterol from the arteries and transport it to the liver for processing. High levels of HDL cholesterol can help lower the risk of heart disease.
Role of Cholesterol in the Body, Best diet to reduce cholesterol
Cholesterol plays a crucial role in various bodily functions, including:
- Cell Membrane Formation: Cholesterol is a vital component of cell membranes, providing structural integrity and regulating the permeability of the cell.
- Hormone Production: Cholesterol is a precursor for the production of essential hormones like estrogen, testosterone, and cortisol, which regulate various bodily functions.
- Vitamin D Synthesis: When exposed to sunlight, the skin converts cholesterol into vitamin D, essential for bone health and calcium absorption.
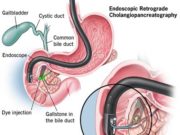
- Digestion and Absorption of Fats: Bile acids, produced from cholesterol, aid in the digestion and absorption of fats in the intestines.
Health Risks Associated with High Cholesterol
High levels of LDL cholesterol can lead to several health problems, including:
- Atherosclerosis: The buildup of plaque in the arteries, restricting blood flow and increasing the risk of heart disease and stroke.
- Heart Disease: High cholesterol contributes to the formation of blood clots, which can block arteries and lead to heart attacks.
- Stroke: When a blood clot blocks an artery in the brain, it can cause a stroke, leading to brain damage and disability.
- Peripheral Artery Disease (PAD): Plaque buildup in the arteries of the legs and feet can restrict blood flow, causing pain, numbness, and even amputation.
Dietary Strategies for Lowering Cholesterol
You can significantly impact your cholesterol levels through dietary changes. This involves making smart food choices to reduce the intake of unhealthy fats while incorporating foods that promote heart health.
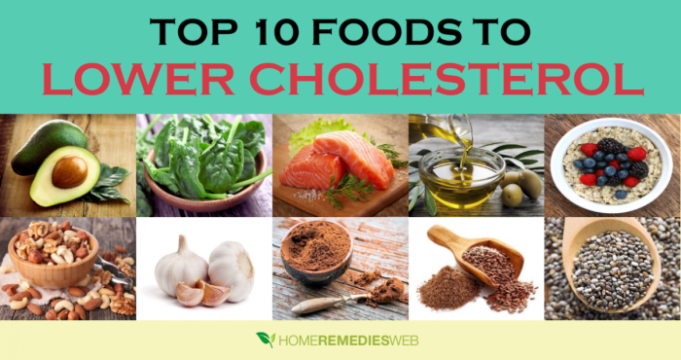
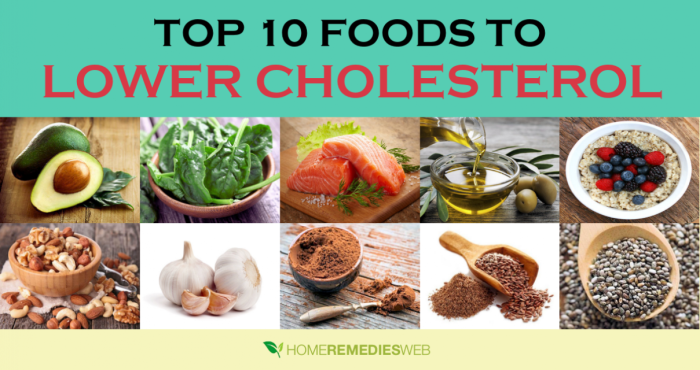
Foods to Include for Lowering Cholesterol
These foods are your allies in the fight against high cholesterol:
- Oily Fish: Salmon, mackerel, tuna, and sardines are rich in omega-3 fatty acids, which have been shown to reduce LDL (bad) cholesterol and increase HDL (good) cholesterol. Aim for at least two servings of oily fish per week.
- Nuts and Seeds: Almonds, walnuts, flaxseeds, and chia seeds are packed with healthy fats, fiber, and antioxidants. They can help lower LDL cholesterol and improve heart health.
- Legumes: Beans, lentils, and peas are excellent sources of fiber, protein, and other nutrients. They can help lower LDL cholesterol and improve blood sugar control.
- Fruits and Vegetables: Fruits and vegetables, particularly those rich in soluble fiber like apples, pears, berries, and Brussels sprouts, can help bind cholesterol in the gut and prevent its absorption into the bloodstream.
- Whole Grains: Whole grains like brown rice, quinoa, and oats provide soluble fiber, which helps lower LDL cholesterol. Opt for whole grain bread, pasta, and cereals over refined grain products.
- Soy Products: Soybeans and soy products like tofu, tempeh, and soy milk are known to lower LDL cholesterol.
Foods to Limit or Avoid
Certain foods can contribute to high cholesterol levels. Here’s a list of foods to limit or avoid:
- Saturated and Trans Fats: Found in red meat, butter, full-fat dairy products, fried foods, and processed foods, these fats raise LDL cholesterol. Aim for lean meats and low-fat dairy options.
- Cholesterol-Rich Foods: Eggs, shellfish, and organ meats (like liver) are naturally high in cholesterol. While these foods can be part of a balanced diet, moderation is key.
- Processed Foods: Processed foods are often loaded with saturated and trans fats, sodium, and sugar, which can contribute to high cholesterol and other health problems. Opt for whole, unprocessed foods whenever possible.
The Role of Fiber in a Cholesterol-Lowering Diet
Fiber plays a crucial role in reducing cholesterol levels. There are two types of fiber:
- Soluble Fiber: This type of fiber dissolves in water and forms a gel-like substance in the gut, which helps bind cholesterol and prevent its absorption into the bloodstream. Good sources of soluble fiber include oats, beans, lentils, apples, and pears.
- Insoluble Fiber: This type of fiber does not dissolve in water and helps add bulk to stool, promoting regular bowel movements. While it doesn’t directly lower cholesterol, it’s important for overall digestive health. Good sources of insoluble fiber include whole grains, vegetables, and nuts.
A diet rich in soluble fiber can help lower LDL cholesterol by up to 10%.
The Mediterranean Diet for Cholesterol Management
The Mediterranean diet, inspired by the traditional eating patterns of people living in the Mediterranean region, has gained widespread recognition for its potential health benefits, including cholesterol management.
Key Components of the Mediterranean Diet
The Mediterranean diet emphasizes a balance of whole, unprocessed foods, prioritizing plant-based sources. Here are some key components:
- Fruits and Vegetables: Abundant consumption of fresh fruits and vegetables, rich in fiber, vitamins, and antioxidants.
- Whole Grains: Whole grains like brown rice, quinoa, and whole-wheat bread provide complex carbohydrates and fiber.
- Healthy Fats: Olive oil, a primary source of monounsaturated fats, is used liberally for cooking and dressings. Other healthy fats include those found in nuts, seeds, and fatty fish.
- Legumes: Lentils, chickpeas, and beans are excellent sources of protein, fiber, and other nutrients.
- Fish and Seafood: Regular consumption of fatty fish like salmon, tuna, and mackerel, rich in omega-3 fatty acids, is encouraged.
- Poultry and Eggs: Moderate intake of poultry and eggs, with preference for lean cuts and egg whites.
- Dairy: Moderate consumption of low-fat dairy products like yogurt and cheese.
- Red Meat and Processed Foods: Limited consumption of red meat and processed foods, which are high in saturated fat.
- Wine (in moderation): Moderate red wine consumption has been linked to potential health benefits, but it is not essential for the diet.
How the Mediterranean Diet Can Contribute to Lowering Cholesterol Levels
The Mediterranean diet can help lower cholesterol levels through various mechanisms:
- High Fiber Content: The abundance of fruits, vegetables, and whole grains in the Mediterranean diet provides ample fiber, which helps bind to cholesterol in the gut and prevent its absorption into the bloodstream.
- Monounsaturated Fats: Olive oil, a cornerstone of the Mediterranean diet, is rich in monounsaturated fats, which have been shown to improve cholesterol profiles by raising HDL (good) cholesterol and lowering LDL (bad) cholesterol.
- Omega-3 Fatty Acids: Regular consumption of fatty fish provides omega-3 fatty acids, which have anti-inflammatory properties and can contribute to lowering triglyceride levels and improving cholesterol profiles.
- Reduced Saturated Fat Intake: The Mediterranean diet emphasizes lean protein sources and limits saturated fat intake from red meat and processed foods, which can help lower LDL cholesterol levels.
Sample Mediterranean Meal Plan for a Week
Here’s a sample Mediterranean meal plan for a week, showcasing the variety and balance of this dietary approach:
Monday
- Breakfast: Oatmeal with berries and a drizzle of olive oil.
- Lunch: Lentil soup with whole-wheat bread and a side salad with vinaigrette dressing.
- Dinner: Grilled salmon with roasted vegetables and quinoa.
Tuesday
- Breakfast: Greek yogurt with fruit and a sprinkle of nuts.
- Lunch: Tuna salad sandwich on whole-wheat bread with lettuce and tomato.
- Dinner: Chicken stir-fry with brown rice and vegetables.
Wednesday
- Breakfast: Whole-wheat toast with avocado and a poached egg.
- Lunch: Chickpea salad with whole-wheat pita bread and a side of fruit.
- Dinner: Vegetarian pasta with marinara sauce and a side of steamed broccoli.
Thursday
- Breakfast: Smoothie with fruit, yogurt, and spinach.
- Lunch: Leftovers from dinner.
- Dinner: Baked chicken breast with roasted sweet potatoes and green beans.
Friday
- Breakfast: Whole-wheat pancakes with berries and a drizzle of maple syrup.
- Lunch: Salad with grilled chicken or fish, mixed greens, and a vinaigrette dressing.
- Dinner: Pizza with whole-wheat crust, vegetables, and a light cheese topping.
Saturday
- Breakfast: Eggs with whole-wheat toast and a side of fruit.
- Lunch: Leftovers from dinner.
- Dinner: Paella with seafood, chicken, and vegetables.
Sunday
- Breakfast: French toast with fruit and a sprinkle of nuts.
- Lunch: Leftovers from dinner.
- Dinner: Roast lamb with roasted vegetables and a side of couscous.
DASH Diet for Cholesterol Reduction
The DASH (Dietary Approaches to Stop Hypertension) diet is a well-regarded dietary pattern that promotes heart health and helps lower cholesterol levels. It’s known for its emphasis on fresh fruits, vegetables, and whole grains, while limiting saturated and unhealthy fats, cholesterol, and sodium.
Key Principles of the DASH Diet
The DASH diet is a balanced approach to eating, focusing on consuming nutrient-rich foods in specific proportions. Here’s a breakdown of its key principles:
- Emphasis on Fruits and Vegetables: The DASH diet encourages a generous intake of fruits and vegetables, providing essential vitamins, minerals, and fiber. Aim for 4-5 servings of fruits and 4-5 servings of vegetables daily.
- Whole Grains Over Refined Grains: Opt for whole grains like brown rice, quinoa, oats, and whole-wheat bread instead of refined grains. Whole grains are rich in fiber, which helps regulate cholesterol levels.
- Lean Protein Sources: Incorporate lean protein sources like poultry without skin, fish, beans, lentils, and low-fat dairy products. These options provide protein without excessive saturated fat.
- Healthy Fats: Limit saturated and trans fats, and prioritize healthy fats like those found in olive oil, avocados, nuts, and seeds. These fats contribute to heart health and can help lower LDL cholesterol.
- Sodium Reduction: The DASH diet emphasizes reducing sodium intake to manage blood pressure. Aim for less than 2,300 milligrams of sodium per day, ideally even lower at 1,500 milligrams for most adults.
Comparison of DASH and Mediterranean Diets
The DASH and Mediterranean diets share similarities in their focus on healthy eating patterns, but they have some key differences:
| Feature | DASH Diet | Mediterranean Diet |
|---|---|---|
| Emphasis | Lowering blood pressure | Heart health, overall well-being |
| Sodium | Strong emphasis on reducing sodium | Less strict on sodium intake |
| Fats | Focuses on reducing saturated and trans fats | Promotes healthy fats like olive oil and avocados |
| Dairy | Recommends low-fat dairy products | Includes full-fat dairy products in moderation |
| Red Meat | Limits red meat intake | Allows red meat in moderation, typically once a week |
Recommended Daily Intake for the DASH Diet
The DASH diet provides specific recommendations for the daily intake of various food groups. Here’s a table outlining these recommendations:
| Food Group | Recommended Daily Servings |
|---|---|
| Fruits | 4-5 servings |
| Vegetables | 4-5 servings |
| Grains | 6-8 servings |
| Lean Meats, Poultry, Fish, Beans, Nuts, and Seeds | 2-3 servings |
| Low-Fat Dairy Products | 2-3 servings |
| Fats and Oils | 2-3 servings |
Beyond Diet
While diet plays a crucial role in cholesterol management, it’s equally important to adopt a holistic approach that incorporates lifestyle modifications. These changes can significantly enhance your efforts to lower cholesterol levels and improve your overall health.
Regular Physical Activity
Engaging in regular physical activity is a powerful tool for lowering cholesterol levels. Exercise helps increase the body’s sensitivity to insulin, leading to improved glucose metabolism and a reduction in the production of harmful LDL cholesterol. It also promotes the production of HDL cholesterol, often referred to as “good cholesterol,” which helps remove LDL cholesterol from the bloodstream.
- Aim for at least 30 minutes of moderate-intensity exercise most days of the week. This could include brisk walking, jogging, swimming, cycling, or dancing.
- If you’re new to exercise, start gradually and increase the intensity and duration over time.
- Even short bursts of activity throughout the day can make a difference. Consider taking the stairs instead of the elevator or walking around during your lunch break.
Managing Stress
Stress can have a significant impact on cholesterol levels. When you’re stressed, your body releases hormones that can increase the production of LDL cholesterol and lower HDL cholesterol.
- Find healthy ways to manage stress, such as yoga, meditation, deep breathing exercises, spending time in nature, or listening to calming music.
- Prioritize sleep and ensure you get at least 7-8 hours of quality sleep each night.
- Engage in activities that you enjoy and find relaxing.
- Practice mindfulness and focus on the present moment.
Maintaining a Healthy Weight
Excess weight can contribute to high cholesterol levels. Losing even a small amount of weight can make a significant difference in lowering your cholesterol.
- Adopt a balanced diet that emphasizes fruits, vegetables, whole grains, and lean protein sources.
- Limit your intake of saturated and trans fats, as well as added sugars.
- Regular physical activity can help you burn calories and maintain a healthy weight.
- Consult with a healthcare professional or registered dietitian to create a personalized weight management plan.
Supplements and Medications for Cholesterol Reduction
While dietary changes are the cornerstone of cholesterol management, certain supplements and medications can play a supportive role. These interventions can help lower cholesterol levels and reduce the risk of heart disease.
Supplements for Cholesterol Reduction
Several supplements have been investigated for their potential to lower cholesterol levels. While some research suggests benefits, more evidence is needed to confirm their effectiveness and safety.
It’s important to consult with a healthcare professional before taking any supplements, especially if you have underlying medical conditions or are taking other medications.
- Plant Sterols and Stanols: These compounds, found naturally in plants, can block the absorption of cholesterol in the gut. Studies have shown that consuming 2 grams daily can lower LDL cholesterol by 5-15%. They are available in various forms, including fortified foods, supplements, and margarines.
- Fiber: Soluble fiber, found in oats, beans, lentils, and fruits, can bind to cholesterol in the gut and prevent its absorption. Aim for 25-30 grams of fiber daily.
- Niacin (Vitamin B3): High doses of niacin can lower LDL cholesterol and raise HDL cholesterol. However, it can cause side effects such as flushing, headaches, and liver problems. Consult your doctor before taking niacin supplements.
- Garlic: Some studies suggest that garlic may have cholesterol-lowering properties. However, the evidence is mixed, and more research is needed.
- Omega-3 Fatty Acids: Found in fatty fish like salmon, tuna, and mackerel, omega-3 fatty acids can lower triglycerides and slightly increase HDL cholesterol.
Statins and Other Medications
Statins are the most commonly prescribed medications for lowering cholesterol. They work by inhibiting an enzyme in the liver that produces cholesterol. Statins have been shown to effectively reduce LDL cholesterol levels and lower the risk of heart disease.
- Statins: Common statins include atorvastatin (Lipitor), simvastatin (Zocor), rosuvastatin (Crestor), and pravastatin (Pravachol). They are generally well-tolerated, but potential side effects include muscle pain, liver problems, and increased risk of diabetes in some individuals.
- Other Medications: Other medications used to manage high cholesterol include:
- Bile acid sequestrants: These medications bind to bile acids in the gut, preventing their reabsorption and leading to increased cholesterol excretion. Examples include cholestyramine (Questran) and colestipol (Colestid).
- Fibrates: These medications lower triglycerides and increase HDL cholesterol. Examples include gemfibrozil (Lopid) and fenofibrate (Tricor).
- Ezetimibe (Zetia): This medication inhibits the absorption of cholesterol from the gut. It is often used in combination with statins.
- PCSK9 inhibitors: These medications block a protein that removes LDL cholesterol from the bloodstream. Examples include alirocumab (Praluent) and evolocumab (Repatha). They are injected and can significantly lower LDL cholesterol levels.
Side Effects and Interactions of Cholesterol-Lowering Medications
Cholesterol-lowering medications can cause side effects, and they may interact with other medications. It’s crucial to discuss potential risks and benefits with your healthcare provider before starting any medication.
- Statins: Common side effects of statins include muscle pain, fatigue, and digestive problems. In rare cases, they can cause liver damage or increase the risk of diabetes.
- Bile Acid Sequestrants: These medications can cause constipation, bloating, and gas.
- Fibrates: Potential side effects of fibrates include muscle pain, stomach upset, and gallstones.
- Ezetimibe: This medication is generally well-tolerated, but some people may experience diarrhea or abdominal pain.
- PCSK9 Inhibitors: These medications can cause injection site reactions and may increase the risk of allergic reactions.
It’s important to note that this information is for general knowledge and should not be considered medical advice. Always consult with your doctor or a qualified healthcare professional for personalized guidance on cholesterol management and medication choices.
Last Point
By understanding the science behind cholesterol and adopting a holistic approach that encompasses diet, exercise, and lifestyle modifications, you can effectively manage your cholesterol levels and reduce your risk of heart disease. Remember, consulting with a healthcare professional is crucial for personalized advice and monitoring your progress. Take control of your health today and embark on a journey towards a healthier tomorrow.
Common Queries
What are the best foods to lower cholesterol?
Foods rich in soluble fiber, like oats, beans, lentils, and fruits like apples and pears, are particularly effective at lowering cholesterol. Additionally, incorporating fatty fish like salmon, mackerel, and tuna, which are rich in omega-3 fatty acids, can also help.
How long does it take to see results from dietary changes?
It typically takes a few weeks to a few months to see significant changes in cholesterol levels after making dietary modifications. However, individual responses may vary.
Can I lower my cholesterol without medication?
Yes, many people can effectively manage their cholesterol levels through lifestyle changes alone, including diet, exercise, and stress management. However, if your cholesterol levels remain high despite these efforts, your doctor may recommend medication.
What are some common misconceptions about cholesterol?
One common misconception is that all cholesterol is bad. In fact, your body needs cholesterol to function properly. The key is to maintain a healthy balance between good (HDL) and bad (LDL) cholesterol.
A diet rich in fruits, vegetables, and whole grains is often recommended for lowering cholesterol levels. It’s important to remember that cholesterol and triglycerides are closely linked, so understanding how to lower triglycerides with diet is also crucial. You can find detailed information on how to lower triglycerides with diet on this website.
By making smart choices about what you eat, you can effectively manage both your cholesterol and triglyceride levels, leading to a healthier lifestyle overall.
A heart-healthy diet to lower cholesterol can be a great choice for overall well-being. But when you’re breastfeeding, you need to consider the needs of your little one too. A balanced diet rich in fruits, vegetables, and lean protein is key, and you can find more detailed guidance on the best diet when breastfeeding.
Remember, the right diet can support both your health and your baby’s growth, so talk to your doctor or a registered dietitian for personalized advice.
While a balanced diet rich in fruits, vegetables, and whole grains is generally recommended for lowering cholesterol, hospital diets often have specific restrictions. These can vary depending on the patient’s condition, and you can learn more about the types of diet in hospital to better understand how they might impact your cholesterol levels.
Ultimately, the best diet to reduce cholesterol is a personalized one that takes into account your individual needs and medical history.