What causes diabetes? This seemingly simple question hides a complex web of factors, weaving together genetics, lifestyle, environment, and even pregnancy. Diabetes, a chronic condition marked by high blood sugar levels, can take many forms, each with its own unique set of contributing factors.
Let’s embark on a journey to understand the intricate dance of these elements that ultimately leads to this prevalent disease.
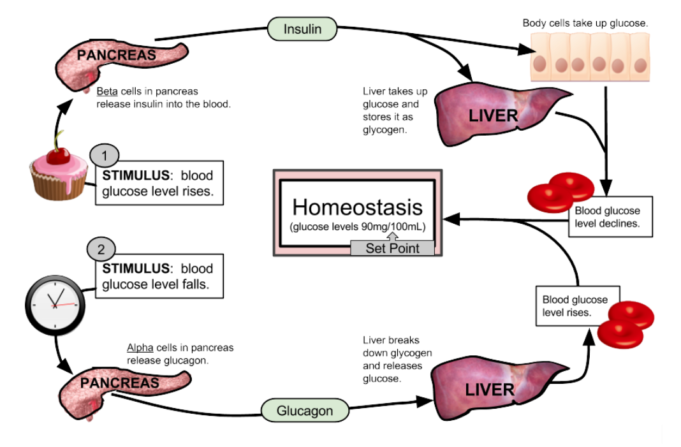
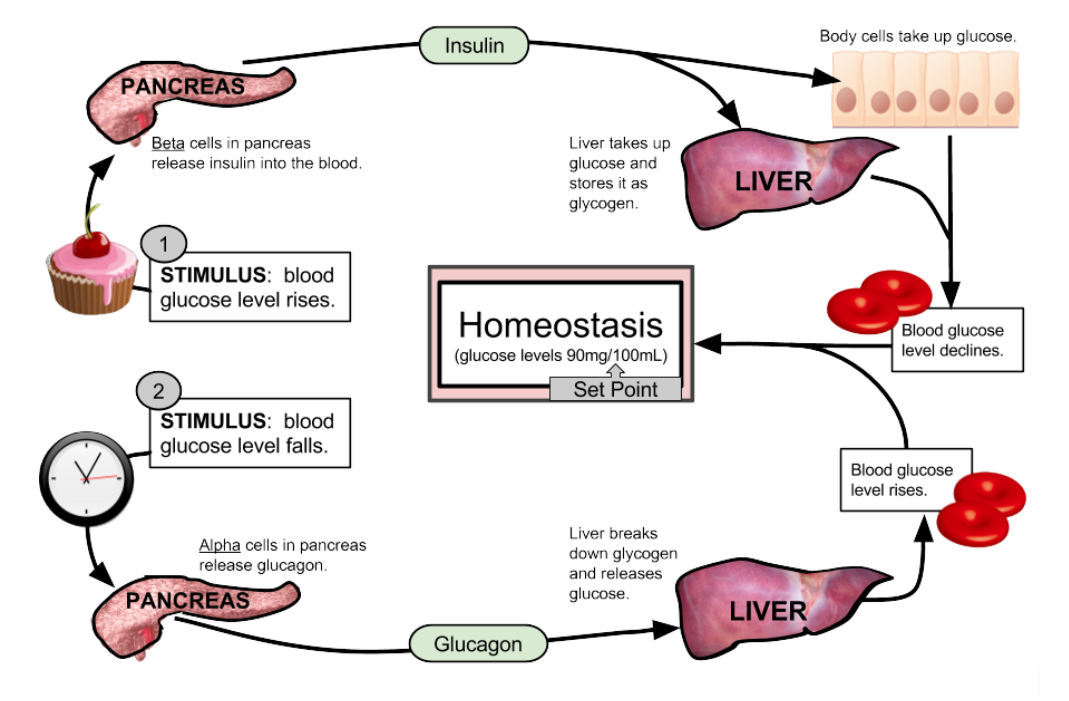
The story of diabetes starts with insulin, a crucial hormone that acts like a key, unlocking cells to let glucose (sugar) enter and provide energy. In type 1 diabetes, the body’s immune system mistakenly attacks the insulin-producing cells, leaving the body unable to regulate blood sugar.
Type 2 diabetes, the more common form, develops when the body becomes resistant to insulin, or the pancreas doesn’t produce enough. Gestational diabetes, a temporary form that develops during pregnancy, adds another layer of complexity, affecting both mother and child.
Understanding Diabetes
Diabetes is a chronic condition that affects how your body regulates blood sugar. It’s like your body’s got a faulty thermostat for glucose, leading to either too much or too little sugar in your bloodstream.
Types of Diabetes
Diabetes comes in different flavors, each with its own unique story.
- Type 1 Diabetes: This is an autoimmune disease where your immune system mistakenly attacks the insulin-producing cells in your pancreas. It’s like your body’s own army is waging war on the very cells that help regulate your blood sugar. This type typically develops in childhood or adolescence, but can occur at any age.
- Type 2 Diabetes: This is the most common type, where your body either doesn’t produce enough insulin or can’t use it properly. It’s like your body’s got a broken insulin key, and the door to your cells won’t open to let the sugar in.Diabetes is a complex condition, often linked to lifestyle choices. While genetics play a role, what you eat and how much you move can be major players in the game. If you’re trying to manage your blood sugar, Tips for avoiding cravings while on a diet can be a lifesaver.Remember, conquering those cravings is like battling a sugar-crazed monster, but with the right strategies, you can win the war against diabetes one sweet tooth at a time!
This type usually develops in adulthood, but is becoming increasingly common in children and adolescents.
- Gestational Diabetes: This type develops during pregnancy and usually goes away after delivery. It’s like your body’s temporarily losing its grip on blood sugar control during pregnancy.
The Role of Insulin
Insulin is the key that unlocks your cells to let glucose (sugar) in. It’s like the bouncer at a nightclub, deciding who gets to enter.
When your blood sugar levels rise after a meal, your pancreas releases insulin, signaling your cells to absorb glucose for energy.
Complications of Uncontrolled Diabetes
If diabetes goes unchecked, it can lead to a whole host of problems, like a party gone wrong.
- Heart Disease and Stroke: High blood sugar can damage blood vessels, making them prone to clogging, increasing the risk of heart attack and stroke.
- Nerve Damage: High blood sugar can damage nerves, leading to numbness, tingling, and pain in the hands, feet, and other parts of the body.
- Kidney Damage: High blood sugar can damage the tiny blood vessels in your kidneys, leading to kidney failure.
- Eye Damage: High blood sugar can damage the blood vessels in your eyes, leading to blurry vision, blindness, and other eye problems.
- Amputations: High blood sugar can impair blood flow to your limbs, leading to infections and possibly amputations.
Genetic Predisposition
Imagine your genes as a blueprint for your body, dictating everything from your hair color to your risk of developing certain diseases. Diabetes, unfortunately, is one such disease where your genetic makeup plays a significant role.
Genes Linked to Increased Diabetes Risk, What causes diabetes
Understanding the specific genes associated with diabetes can help us grasp the complex interplay between genetics and disease. While numerous genes have been linked to an increased risk of developing diabetes, some of the key players include:
- TCF7L2: This gene is heavily involved in regulating insulin secretion, and variations in this gene have been strongly linked to type 2 diabetes.
- PPARG: This gene plays a crucial role in insulin sensitivity, and mutations in this gene have been associated with an increased risk of developing both type 1 and type 2 diabetes.
- KCNJ11: This gene is involved in potassium channel function, which is critical for insulin release. Variations in this gene have been associated with an increased risk of type 2 diabetes.
Role of Family History in Diabetes Risk
It’s often said that “diabetes runs in the family,” and there’s a strong scientific basis for this statement. If your close relatives have diabetes, your risk of developing the disease is significantly higher. This is because you share a significant portion of your genetic makeup with your family members, increasing the likelihood of inheriting genes linked to diabetes.
Genetic Testing for Diabetes Risk Assessment
Genetic testing can provide valuable insights into your personal diabetes risk. These tests analyze your DNA to identify specific gene variations that have been linked to an increased risk of developing diabetes. While genetic testing cannot predict with certainty whether you will develop diabetes, it can help you understand your individual risk and take proactive steps to manage your health.
Lifestyle Factors
While genetics play a role, lifestyle choices can significantly impact your risk of developing diabetes. Think of it like this: your genes might set the stage, but your lifestyle choices are the actors who determine the play’s outcome.
Diet and Nutrition
Your diet is a key player in diabetes prevention. Imagine your body as a car; it needs the right fuel to run smoothly. A diet rich in processed foods, sugary drinks, and unhealthy fats is like pouring low-quality gasoline into your car – it’s going to sputter and eventually break down.
On the other hand, a diet filled with whole grains, fruits, vegetables, and lean protein is like using premium fuel – it keeps your body running efficiently and reduces your risk of developing diabetes.
- Limit sugary drinks: Think soda, fruit punch, and even some fruit juices. These drinks are packed with sugar and contribute to weight gain, a major risk factor for diabetes.
- Choose whole grains: Whole grains like brown rice, quinoa, and whole-wheat bread are packed with fiber, which helps regulate blood sugar levels. They also provide essential nutrients that can help prevent diabetes.
- Load up on fruits and vegetables: Fruits and vegetables are naturally low in calories and high in fiber, making them excellent choices for a diabetes-prevention diet. They also provide vitamins and minerals that are essential for overall health.
- Choose lean protein sources: Lean protein sources like fish, poultry, beans, and tofu are lower in saturated fat and calories, which can help with weight management and reduce diabetes risk.
Maintaining a Healthy Weight
Maintaining a healthy weight is crucial for preventing diabetes. Being overweight or obese puts extra strain on your pancreas, the organ responsible for producing insulin. This strain can lead to insulin resistance, a precursor to type 2 diabetes.
Think of it like this: If you overload your car’s engine, it’s going to struggle to run smoothly. Similarly, if you overload your pancreas with excess weight, it’s going to struggle to produce enough insulin.
- Set realistic weight loss goals: Aim to lose 1-2 pounds per week. This is a healthy and sustainable rate of weight loss. Don’t try to lose weight too quickly, as this can be unhealthy and unsustainable.
- Make gradual changes to your diet: Start by making small changes, like cutting out sugary drinks or adding more fruits and vegetables to your meals. As you get comfortable with these changes, you can gradually make more significant changes.
- Increase your physical activity: Regular physical activity can help you lose weight and improve your insulin sensitivity. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
Regular Physical Activity
Physical activity is like giving your body a tune-up. It helps improve insulin sensitivity, which means your body can use insulin more effectively. This helps keep blood sugar levels in check and reduces your risk of developing diabetes.
Plus, regular exercise can help you maintain a healthy weight, which is another key factor in diabetes prevention.
- Aim for at least 30 minutes of moderate-intensity exercise most days of the week: Moderate-intensity exercise includes activities like brisk walking, swimming, cycling, and dancing. You should be able to talk comfortably while exercising.
- Include strength training in your routine: Strength training helps build muscle mass, which can improve insulin sensitivity. Aim for two strength-training sessions per week.
- Find activities you enjoy: The key to staying active is finding activities you enjoy. If you don’t enjoy what you’re doing, you’re less likely to stick with it. So try different activities until you find something that fits your interests and lifestyle.
Environmental Factors
While genetics and lifestyle play a significant role in diabetes development, the environment we live in also has a considerable impact. Think of it like this: your genes are the blueprint, your lifestyle is the construction crew, and the environment is the weather that can either help or hinder the building process.
Let’s explore some of the environmental factors that can influence your risk of developing diabetes.
Exposure to Environmental Toxins
The modern world is full of toxins, some more obvious than others. From pesticides in our food to air pollution in our cities, our bodies are constantly bombarded with these chemical invaders. And while some toxins might not directly cause diabetes, they can disrupt the delicate balance of our endocrine system, the network of glands that produce hormones like insulin.
This disruption can make our bodies less sensitive to insulin, leading to an increased risk of developing diabetes.
- Pesticides:Studies have linked exposure to certain pesticides, particularly organochlorines, to an increased risk of type 2 diabetes. These chemicals can interfere with insulin signaling and disrupt glucose metabolism.
- Heavy Metals:Exposure to heavy metals like lead and cadmium can also increase diabetes risk. These metals can accumulate in the body and damage the pancreas, the organ responsible for producing insulin.
- Bisphenol A (BPA):This chemical found in many plastic products can disrupt hormone function and has been linked to an increased risk of diabetes in some studies.
Stress and Sleep Deprivation
We all know that stress and sleep deprivation are bad for our health, but did you know they can also increase your risk of diabetes? Think of stress and sleep deprivation as two sneaky saboteurs, quietly chipping away at your body’s defenses against diabetes.
Diabetes, that pesky sugar-loving monster, can be caused by a whole host of factors, including genetics and lifestyle choices. But let’s face it, if you’re carrying around extra weight, it’s like giving diabetes a free pass to wreak havoc on your body.
So, if you’re looking to shed some pounds and give diabetes the boot, check out this awesome resource on diet to lose weight. It might just be the secret weapon you need to keep your blood sugar in check and say “buh-bye” to those pesky diabetes complications.
- Stress:Chronic stress can lead to increased cortisol levels, a hormone that can increase insulin resistance and blood sugar levels. It also can make it harder for your body to regulate blood sugar.
- Sleep Deprivation:When you’re sleep-deprived, your body produces more of the stress hormone cortisol and less of the hormone leptin, which helps regulate appetite. This can lead to increased insulin resistance and weight gain, both of which are risk factors for diabetes.
Air Pollution
You might not think of air pollution as a direct cause of diabetes, but it can have a significant impact on your health. Think of air pollution as a constant assault on your body, making it harder for your cells to function properly.
- Fine Particulate Matter:Tiny particles in polluted air can penetrate deep into your lungs and even enter your bloodstream, triggering inflammation and damaging cells. This inflammation can contribute to insulin resistance and increase your risk of diabetes.
- Ozone:This gas, often found in smog, can damage lung tissue and increase inflammation. Studies have shown a link between ozone exposure and increased risk of type 2 diabetes.
Medical Conditions: What Causes Diabetes
You know how sometimes you get a cold and your body goes into overdrive to fight it off? Well, sometimes your body can get a little overzealous and start attacking its own cells. This can lead to some serious health issues, including diabetes.
Autoimmune Diseases
Autoimmune diseases are like a case of mistaken identity. Your immune system, which normally protects you from invaders like bacteria and viruses, gets confused and starts attacking your own healthy cells. In the case of diabetes, this can happen in the pancreas, where insulin is made.
Diabetes, that pesky condition that makes your blood sugar do a wild dance, can be caused by a few things. Genetics plays a role, and sometimes, it’s just a matter of bad luck. But, if you’re looking for a deeper dive into the “why” behind diabetes, you might want to check out some Keywords that can shed some light on the subject.
After all, understanding the causes can help you take steps to manage it and keep those blood sugar levels in check.
There are two main types of autoimmune diabetes:
- Type 1 Diabetes:This is an autoimmune disease where your immune system attacks the insulin-producing cells in your pancreas. This leads to a lack of insulin, which is crucial for regulating blood sugar levels.
- LADA (Latent Autoimmune Diabetes in Adults):This is a slower-developing form of type 1 diabetes. It often mimics type 2 diabetes, but the underlying cause is still an autoimmune attack on the pancreas.
Pregnancy and Diabetes
Pregnancy can be a rollercoaster ride of emotions, hormonal changes, and cravings for pickles and ice cream. But for some women, it also comes with an unexpected passenger: diabetes. This is where gestational diabetes, a type of diabetes that develops during pregnancy, enters the picture.
Gestational Diabetes Development
Gestational diabetes occurs when the body doesn’t produce enough insulin to meet the increased demands of pregnancy. This usually happens in the second or third trimester, when the placenta produces hormones that interfere with the body’s ability to use insulin effectively.
It’s like the body’s saying, “Hold my insulin, I’m going to go on a sugar-fueled adventure!”
Risks of Gestational Diabetes
Gestational diabetes isn’t just a pregnancy complication; it can have potential risks for both mom and baby.
Risks for Mom
- High Blood Pressure:Think of it as a battle between your blood sugar and your blood pressure, and gestational diabetes often wins the first round. This can lead to preeclampsia, a serious condition that can affect both mom and baby.
- Premature Birth:Imagine a tiny baby wanting to enter the world early. Gestational diabetes can increase the risk of preterm labor, which can lead to complications for the baby.
- C-section:Sometimes, a baby’s size or other factors related to gestational diabetes can make a vaginal delivery more challenging, leading to a C-section.
- Increased Risk of Type 2 Diabetes:Gestational diabetes can be a sneak peek into the future. Women who have had gestational diabetes have a higher chance of developing type 2 diabetes later in life.
Risks for Baby
- Macrosomia:This means a big baby! High blood sugar can lead to the baby growing larger than average, which can make delivery more difficult.
- Hypoglycemia:Imagine a baby’s blood sugar taking a roller coaster ride! After birth, babies born to mothers with gestational diabetes can experience low blood sugar.
- Respiratory Distress Syndrome:This is when a baby’s lungs aren’t fully developed and they have trouble breathing. Gestational diabetes can increase the risk of this condition.
- Increased Risk of Childhood Obesity:Babies born to mothers with gestational diabetes may have a higher chance of becoming obese later in life.
Managing Gestational Diabetes
Managing gestational diabetes is like a dance between your body and your doctor. It involves a combination of lifestyle changes and sometimes medication.
Lifestyle Changes
- Healthy Diet:Think of it as a delicious journey of balanced meals and snacks that keep your blood sugar in check. This includes plenty of fruits, vegetables, whole grains, and lean proteins.
- Regular Exercise:Get your body moving with regular exercise. It’s like giving your insulin a high-five and telling it to do its job.
- Blood Sugar Monitoring:Regularly checking your blood sugar levels is like keeping an eye on the speedometer of your pregnancy journey.
Medication
- Insulin:Sometimes, your body needs a little extra help from insulin to keep blood sugar levels stable. This is like giving your body a boost to get things moving smoothly.
Prevention Strategies
While you can’t always control your genes, you can take steps to lower your risk of developing diabetes. Prevention strategies focus on lifestyle modifications that can significantly impact your overall health and well-being.
Lifestyle Modifications for Diabetes Prevention
Lifestyle modifications play a crucial role in preventing diabetes. By adopting healthy habits, you can reduce your risk and improve your overall health. Here’s a table summarizing key lifestyle changes:
| Category | Recommendations |
|---|---|
| Diet |
|
| Exercise |
|
| Weight Management |
|
| Stress Reduction |
|
Healthy Food Choices
Making smart food choices is essential for preventing diabetes. Here are some examples of healthy foods to incorporate into your diet:
- Fruits:Apples, bananas, berries, oranges, pears
- Vegetables:Broccoli, carrots, spinach, sweet potatoes, tomatoes
- Lean Proteins:Chicken, fish, beans, lentils, tofu
- Whole Grains:Brown rice, quinoa, whole-wheat bread, oatmeal
- Healthy Fats:Olive oil, avocado, nuts, seeds
Incorporating Physical Activity
Regular physical activity is crucial for diabetes prevention. Here are some tips for incorporating exercise into your daily routine:
- Take the stairs instead of the elevator.
- Walk or bike to work or errands.
- Park further away from your destination and walk the rest of the way.
- Join a gym or fitness class.
- Find an activity you enjoy, like dancing, swimming, or hiking.
- Make exercise a social activity by joining a running group or taking a fitness class with friends.
Concluding Remarks
Understanding what causes diabetes is essential for preventing and managing this condition. While some factors are beyond our control, such as genetics, others, like lifestyle choices, are within our grasp. By embracing healthy habits, we can empower ourselves to reduce our risk and take charge of our well-being.
From the intricate dance of genes to the impact of our daily choices, the story of diabetes unfolds, reminding us that knowledge is power, and prevention is key.
Question & Answer Hub
Is diabetes contagious?
No, diabetes is not contagious. It’s not caused by a virus or bacteria that can spread from person to person.
Can diabetes be reversed?
While diabetes can’t be completely reversed, some people with type 2 diabetes can achieve remission through significant lifestyle changes, including weight loss and exercise.
What are the early signs of diabetes?
Early signs can include increased thirst, frequent urination, excessive hunger, unexplained weight loss, fatigue, blurred vision, and slow-healing sores.
Can I prevent diabetes if I have a family history of it?
While a family history of diabetes increases your risk, it doesn’t guarantee you’ll develop it. Making healthy lifestyle choices can significantly reduce your risk.