What diet for IBS? It’s a question many people with irritable bowel syndrome (IBS) ask. IBS is a common disorder that affects the large intestine, causing symptoms like abdominal pain, bloating, gas, diarrhea, and constipation. While there’s no cure for IBS, dietary changes can significantly improve symptoms.
This guide explores various dietary approaches for IBS, including the low FODMAP diet, gluten-free diet, and Mediterranean diet. We’ll also discuss lifestyle modifications that can help manage IBS symptoms, such as regular exercise, stress management, and adequate sleep.
Understanding Irritable Bowel Syndrome (IBS)
Irritable bowel syndrome (IBS) is a common disorder that affects the large intestine. It causes a variety of symptoms, including abdominal pain, cramping, bloating, gas, diarrhea, and constipation. IBS is a chronic condition, meaning it can last for a long time. However, there are ways to manage the symptoms and improve your quality of life.
Types of IBS
IBS is classified into different types based on the predominant symptoms:
- IBS with diarrhea (IBS-D): This type is characterized by frequent loose stools, often accompanied by urgency and abdominal pain.
- IBS with constipation (IBS-C): This type is characterized by infrequent bowel movements, hard stools, and difficulty passing stool.
- IBS with mixed bowel habits (IBS-M): This type is characterized by alternating periods of diarrhea and constipation.
- Unspecified IBS: This category is used when symptoms don’t fit neatly into the other categories.
Causes and Risk Factors, What diet for ibs
The exact cause of IBS is unknown, but it’s believed to be a combination of factors, including:
- Gastrointestinal motility problems: The muscles in the intestines may not be working properly, leading to irregular contractions and altered bowel movements.
- Increased intestinal sensitivity: The nerves in the gut may be overly sensitive, leading to pain and discomfort even in response to normal bowel movements.
- Gut microbiome imbalances: The balance of bacteria in the gut may be disrupted, contributing to IBS symptoms.
- Psychological factors: Stress, anxiety, and depression can worsen IBS symptoms.
- Food sensitivities: Some people with IBS may experience symptoms after consuming certain foods, such as dairy, gluten, or spicy foods.
- Infections: Past gastrointestinal infections can sometimes trigger IBS.
- Family history: IBS has been shown to run in families, suggesting a genetic component.
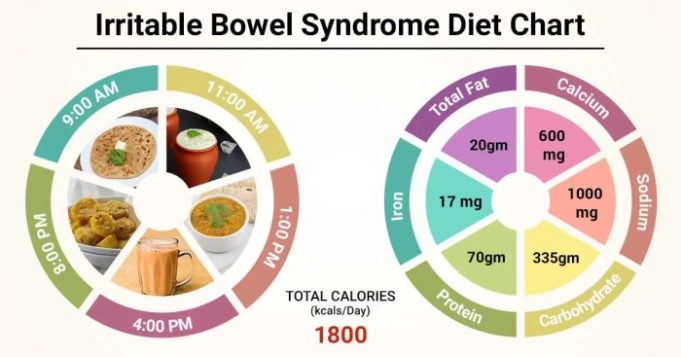
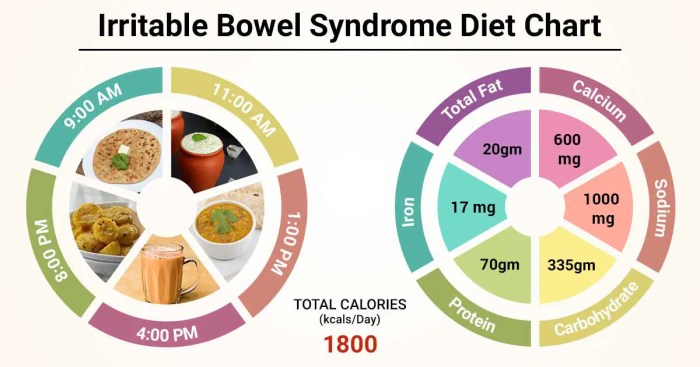
General Dietary Recommendations for IBS
While there’s no one-size-fits-all diet for IBS, following a few general dietary recommendations can help manage symptoms. These recommendations focus on promoting digestive health and minimizing triggers that worsen IBS.
Regular Meals and Adequate Hydration
Eating regular meals throughout the day helps prevent fluctuations in blood sugar levels, which can contribute to IBS symptoms. Skipping meals can lead to increased stomach acid production and exacerbate discomfort. Adequate hydration is crucial for maintaining proper digestion and bowel function. Aim for 8 glasses of water per day, and consider consuming clear broths or herbal teas.
Identifying and Avoiding Trigger Foods
Identifying trigger foods that worsen IBS symptoms is crucial for effective management. Common trigger foods include:
- High-fat foods: Fatty foods can slow down digestion and increase bloating and gas. Examples include fried foods, fatty meats, and dairy products.
- Fiber-rich foods: While fiber is essential for digestive health, excessive intake can worsen IBS symptoms. Examples include beans, lentils, and whole grains.
- Spicy foods: Spicy foods can irritate the digestive tract, leading to diarrhea and abdominal pain. Examples include chili peppers, hot sauce, and curry.
- Carbonated drinks: Carbonation can contribute to bloating and gas. Examples include soda, sparkling water, and beer.
- Alcohol: Alcohol can irritate the digestive system and worsen IBS symptoms.
- Caffeine: Caffeine can stimulate bowel movements and increase diarrhea. Examples include coffee, tea, and chocolate.
Keep a food diary to track your meals and note any symptoms you experience. This will help you identify patterns and pinpoint specific trigger foods.
The Low FODMAP Diet
The Low FODMAP diet is a dietary approach designed to reduce symptoms of Irritable Bowel Syndrome (IBS) by limiting the intake of certain types of carbohydrates known as FODMAPs (Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols).
FODMAPs are short-chain carbohydrates that are poorly absorbed in the small intestine, leading to fermentation by gut bacteria. This fermentation process can produce gas, bloating, and other symptoms commonly experienced by individuals with IBS. By restricting FODMAPs, the Low FODMAP diet aims to reduce the amount of fermentation in the gut and alleviate these symptoms.
Common FODMAP Foods and Low FODMAP Alternatives
Understanding which foods contain high amounts of FODMAPs is crucial for successfully implementing the Low FODMAP diet.
Here are some examples of common high FODMAP foods and their low FODMAP alternatives:
High FODMAP Foods
- Fruits: Apples, pears, watermelon, mango, cherries, peaches, plums, apricots, and dried fruits like raisins and dates.
- Vegetables: Asparagus, artichokes, onions, garlic, leeks, beans, lentils, and mushrooms.
- Dairy: Milk, yogurt, ice cream, and soft cheeses.
- Grains: Wheat, rye, and barley.
- Sweeteners: Honey, agave nectar, and high-fructose corn syrup.
- Other: Sugar-free gum, artificial sweeteners like sorbitol and mannitol, and some processed foods containing high FODMAP ingredients.
Low FODMAP Alternatives
- Fruits: Berries (strawberries, blueberries, raspberries), bananas (in moderation), and citrus fruits (oranges, grapefruits, lemons, limes).
- Vegetables: Carrots, zucchini, spinach, lettuce, broccoli, and cauliflower.
- Dairy: Lactose-free milk, lactose-free yogurt, hard cheeses (cheddar, Swiss, Parmesan), and goat’s milk products.
- Grains: Gluten-free bread, rice, quinoa, and corn.
- Sweeteners: Stevia, erythritol, and monk fruit.
- Other: Sugar-free gum with low FODMAP sweeteners, and processed foods that are specifically labeled as low FODMAP.
Working with a Healthcare Professional
It is essential to consult with a healthcare professional or registered dietitian before starting the Low FODMAP diet. They can provide personalized guidance, assess your individual needs, and ensure the diet is safe and effective for you.
The Low FODMAP diet is a restrictive diet that should be followed under the supervision of a healthcare professional. It is not a long-term solution for IBS and may not be suitable for everyone.
Other Dietary Approaches for IBS: What Diet For Ibs
While the Low FODMAP diet is a widely recognized approach for IBS, other dietary strategies might be helpful for certain individuals. These approaches often target specific dietary components or promote overall gut health.
The Gluten-Free Diet
The gluten-free diet eliminates gluten, a protein found in wheat, barley, and rye. Some people with IBS experience symptom improvement on a gluten-free diet, even if they don’t have celiac disease. While the exact mechanisms are not fully understood, gluten may trigger inflammation or alter gut bacteria in susceptible individuals. However, it’s important to note that the gluten-free diet is not universally effective for IBS, and a proper diagnosis is crucial before adopting this approach.
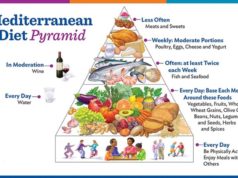
The Mediterranean Diet
The Mediterranean diet emphasizes fruits, vegetables, whole grains, legumes, nuts, seeds, olive oil, and fish, while limiting red meat, processed foods, and saturated fats. This diet pattern promotes overall gut health and may be beneficial for IBS due to its high fiber content and anti-inflammatory properties. Fiber, particularly soluble fiber, can help regulate bowel movements and reduce symptoms of diarrhea and constipation. Additionally, the antioxidants and polyphenols found in Mediterranean foods may contribute to reducing inflammation in the gut.
Other Dietary Approaches
Other dietary approaches, while not as widely studied as the Low FODMAP or gluten-free diets, may provide relief for some individuals with IBS.
The BRAT Diet
The BRAT diet, which stands for bananas, rice, applesauce, and toast, is often recommended for acute diarrhea. It provides a bland, easily digestible source of carbohydrates and electrolytes. While it can be helpful in the short term, the BRAT diet is not a long-term solution for IBS and may lead to nutritional deficiencies if followed for extended periods.
Lifestyle Modifications for IBS Management
Beyond dietary changes, incorporating lifestyle modifications can significantly contribute to managing IBS symptoms and improving overall well-being.
Regular Physical Activity and Stress Management
Regular physical activity plays a crucial role in IBS management. Exercise can help regulate bowel movements, reduce stress levels, and improve mood. Aim for at least 30 minutes of moderate-intensity exercise most days of the week. Activities like brisk walking, swimming, cycling, or yoga are excellent options.
Stress management techniques are equally important. Chronic stress can exacerbate IBS symptoms. Incorporating relaxation techniques such as deep breathing exercises, meditation, or mindfulness into your daily routine can help reduce stress and its impact on your digestive system.
Sleep Quality and IBS
Sleep quality is directly linked to IBS symptoms. When you’re sleep-deprived, your body produces more of the stress hormone cortisol, which can trigger IBS flare-ups. Aim for 7-8 hours of quality sleep each night.
Tips for Improving Sleep Hygiene
- Establish a regular sleep schedule, going to bed and waking up around the same time each day, even on weekends.
- Create a relaxing bedtime routine that helps signal your body it’s time to sleep. This could include taking a warm bath, reading a book, or listening to calming music.
- Make sure your bedroom is dark, quiet, and cool. Avoid using electronic devices in bed, as the blue light emitted from these devices can interfere with sleep.
- Avoid caffeine and alcohol before bed, as they can disrupt sleep patterns.
Probiotics and Prebiotics for IBS
Probiotics are live bacteria that are beneficial for gut health. They can help restore the balance of bacteria in the gut, which can be disrupted in individuals with IBS. Prebiotics, on the other hand, are types of fiber that act as food for the beneficial bacteria in the gut. They promote the growth and activity of these bacteria, contributing to a healthy gut microbiome.
Potential Benefits of Probiotics and Prebiotics for IBS
- Reduced symptoms: Studies have shown that probiotics may help reduce the frequency and severity of IBS symptoms, including abdominal pain, bloating, and diarrhea.
- Improved gut health: Both probiotics and prebiotics can contribute to a healthier gut microbiome, which is essential for overall well-being.
- Reduced inflammation: Some probiotics have anti-inflammatory properties, which may help reduce inflammation in the gut, a common factor in IBS.
Seeking Professional Guidance
Navigating the complexities of Irritable Bowel Syndrome (IBS) can be challenging, and seeking professional guidance is crucial for effective management. Consulting with a healthcare professional is essential for a personalized diagnosis and treatment plan tailored to your individual needs.
The Role of a Registered Dietitian
Registered dietitians are qualified healthcare professionals specializing in nutrition. They play a vital role in developing personalized dietary plans for individuals with IBS. By understanding your specific symptoms and triggers, a registered dietitian can help you identify foods to avoid or limit and recommend dietary modifications that promote gut health and alleviate discomfort.
- They can help you identify and eliminate potential food triggers, such as high-FODMAP foods, which are known to cause digestive distress in many individuals with IBS.
- Registered dietitians can guide you on incorporating nutrient-rich foods into your diet, ensuring you receive the necessary vitamins and minerals for overall well-being.
- They can provide practical advice on meal planning, portion control, and hydration strategies to manage IBS symptoms effectively.
The Benefits of Seeking Support from a Therapist or Counselor
IBS can significantly impact mental health, often leading to stress, anxiety, and depression. Seeking support from a therapist or counselor can provide valuable tools and strategies for managing these emotional challenges.
- Therapy can help you develop coping mechanisms for dealing with IBS-related stress and anxiety, promoting a more positive and resilient outlook.
- Therapists can guide you in understanding the connection between your mental and physical health, empowering you to manage IBS symptoms more effectively.
- They can provide a safe and supportive space to discuss your concerns and explore strategies for reducing stress and improving your overall well-being.
Final Conclusion
Managing IBS often involves a combination of dietary adjustments, lifestyle changes, and professional guidance. While the journey can be challenging, understanding your triggers and adopting a personalized approach can lead to significant symptom relief. Remember, seeking professional advice from a healthcare provider or registered dietitian is crucial for creating a safe and effective plan tailored to your individual needs.
Query Resolution
Can I cure IBS with diet alone?
While diet can significantly improve symptoms, it’s important to understand that there is no cure for IBS. Dietary changes can help manage symptoms and improve quality of life, but it’s essential to consult with a healthcare professional for personalized advice and diagnosis.
How long does it take to see results from dietary changes for IBS?
The time it takes to see results varies depending on the individual and the specific dietary changes made. Some people may notice improvements within a few days or weeks, while others may take longer. It’s crucial to be patient and consistent with dietary changes to see the best results.
Are there any foods I should always avoid with IBS?
Trigger foods vary from person to person. It’s important to identify your individual triggers through a food diary or working with a registered dietitian. Common trigger foods include high-FODMAP foods, gluten, dairy, and spicy foods.
What are probiotics and how can they help with IBS?
Probiotics are live bacteria that are beneficial for gut health. Some research suggests that probiotics may help improve IBS symptoms by restoring balance to the gut microbiome. Probiotics are found in fermented foods like yogurt, sauerkraut, and kimchi, or as supplements.