What diet with diverticulitis takes center stage as we delve into the world of managing this common digestive condition. Diverticulitis, characterized by inflammation or infection of small pouches that form in the lining of the colon, can be a source of discomfort and concern. Understanding the role of diet in preventing and managing diverticulitis is crucial for improving your overall well-being.
This guide will explore the intricacies of diet and diverticulitis, providing valuable insights into the foods that can help alleviate symptoms and promote healing. We will discuss the importance of fiber intake, the benefits of a low-residue diet during flare-ups, and the long-term benefits of a high-fiber diet. Additionally, we will address the role of hydration, lifestyle modifications, and the potential use of dietary supplements.
Understanding Diverticulitis
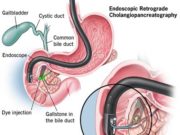
Diverticulitis is a common condition that affects the digestive system. It occurs when small, pouch-like sacs called diverticula form in the lining of the colon, the large intestine. These sacs can become inflamed or infected, leading to a painful condition known as diverticulitis.
Causes of Diverticulitis
Diverticulitis is often associated with a low-fiber diet, which can lead to increased pressure in the colon. This pressure can cause the lining of the colon to bulge outward, forming diverticula. Other factors that may contribute to the development of diverticulitis include:
- Age: The risk of diverticulitis increases with age, as the colon becomes weaker and more prone to bulging.
- Genetics: People with a family history of diverticulitis may be at an increased risk.
- Obesity: Being overweight or obese can increase the pressure in the colon.
- Smoking: Smoking can damage the lining of the colon and increase the risk of diverticulitis.
- Certain medications: Some medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), may increase the risk of diverticulitis.
Symptoms of Diverticulitis
The symptoms of diverticulitis can vary depending on the severity of the condition. Some common symptoms include:
- Abdominal pain: This is usually located in the lower left abdomen and may be severe.
- Fever: A fever is a common sign of infection.
- Nausea and vomiting: These symptoms may occur due to the inflammation in the colon.
- Diarrhea or constipation: Changes in bowel habits are common.
- Blood in the stool: This may occur if the diverticula have ruptured or if there is bleeding in the colon.
Complications of Diverticulitis
If left untreated, diverticulitis can lead to serious complications, including:
- Abscess: A collection of pus may form near the inflamed diverticula, requiring drainage.
- Peritonitis: The infection may spread to the lining of the abdomen, causing a life-threatening condition.
- Fistula: A connection may form between the colon and another organ, such as the bladder or small intestine.
- Obstruction: The inflamed diverticula may block the colon, causing a bowel obstruction.
- Bleeding: The diverticula may bleed, causing blood in the stool.
The Role of Diet in Diverticulitis Management
Diet plays a crucial role in managing diverticulitis, a condition that affects the digestive system. Understanding the impact of food on this condition is essential for preventing flare-ups and promoting long-term health.
Fiber Intake and Diverticulitis
Fiber is a crucial component of a healthy diet, particularly for individuals with diverticulitis. It’s essential for maintaining regular bowel movements and preventing constipation, which can contribute to the development of diverticula—small pouches that can form in the colon wall.
While fiber is generally beneficial, it’s important to note that high-fiber diets can sometimes trigger diverticulitis flare-ups, especially during acute episodes. During these periods, doctors often recommend a low-fiber diet to allow the inflamed colon to rest and heal. However, once the flare-up subsides, gradually increasing fiber intake is essential for preventing future episodes.
High-Fiber Foods for Diverticulitis
A high-fiber diet is generally recommended for individuals with diverticulitis to prevent future flare-ups. Here are some examples of high-fiber foods that are beneficial:
- Fruits: Apples (with skin), pears, berries, bananas, oranges, and grapefruit.
- Vegetables: Broccoli, Brussels sprouts, carrots, spinach, peas, and sweet potatoes.
- Grains: Whole-wheat bread, brown rice, oatmeal, quinoa, and barley.
- Legumes: Beans (kidney, black, pinto), lentils, and chickpeas.
- Nuts and Seeds: Almonds, walnuts, sunflower seeds, and flax seeds.
Low-Fiber Foods to Avoid During Flare-Ups
During an acute diverticulitis flare-up, it’s essential to follow a low-fiber diet to minimize irritation and promote healing. Here are some examples of low-fiber foods to avoid:
| Food Category | Examples |
|---|---|
| Fruits | Bananas (ripe), watermelon, cantaloupe, cooked applesauce, and cooked pears |
| Vegetables | Cooked carrots, cooked spinach, cooked squash, and cooked asparagus |
| Grains | White bread, white rice, and pasta |
| Other | Dairy products, eggs, lean meats, and fish |
The Low-Residue Diet: What Diet With Diverticulitis
The low-residue diet is a dietary approach often recommended for individuals experiencing diverticulitis. This diet aims to reduce the amount of fiber and undigested food particles in the colon, minimizing irritation and promoting healing.
Purpose and Principles of the Low-Residue Diet
The low-residue diet focuses on limiting the intake of foods that produce a high volume of undigested material in the colon. This approach helps to decrease the pressure within the colon, potentially reducing the risk of further diverticulitis episodes.
The low-residue diet aims to reduce the amount of fiber and undigested food particles in the colon, minimizing irritation and promoting healing.
Sample Meal Plan for a Low-Residue Diet
A sample meal plan for a low-residue diet includes:
Breakfast
- Scrambled eggs with cooked, diced ham
- Oatmeal made with water (avoid adding fruit or nuts)
- Plain yogurt with honey or a small amount of fruit
Lunch
- Grilled chicken breast with cooked vegetables like carrots or zucchini
- Tuna salad sandwich on white bread (avoid whole-grain bread)
- Soup made with broth and finely chopped vegetables
Dinner
- Baked cod with mashed potatoes and steamed green beans
- Chicken stir-fry with white rice (avoid high-fiber vegetables like broccoli)
- Lentil soup made with well-cooked lentils and broth (avoid whole lentils)
Foods to Avoid During a Low-Residue Diet
During a low-residue diet, it’s crucial to avoid foods that are high in fiber and difficult to digest. This includes:
- Raw fruits and vegetables (including berries, apples, pears, and broccoli)
- Whole grains (such as brown rice, quinoa, and whole-wheat bread)
- Seeds and nuts
- Dried beans and legumes
- Popcorn
- Corn
- Tough meats (such as steak and pork chops)
- Spicy foods
- High-fat foods
The High-Fiber Diet
While a low-residue diet is crucial during acute diverticulitis, a high-fiber diet is vital for long-term prevention and management. It promotes healthy bowel function, strengthens the colon’s muscles, and reduces the risk of diverticulitis recurrence.
Increasing Fiber Intake Gradually
It’s crucial to increase fiber intake gradually to avoid discomfort and potential complications. Starting with a low-fiber diet and gradually adding more fiber-rich foods allows your digestive system to adjust and adapt.
A gradual increase in fiber intake can help prevent symptoms like bloating, gas, and constipation, which are common when transitioning to a high-fiber diet. It’s also important to stay hydrated by drinking plenty of water, as this helps fiber move through the digestive system smoothly.
High-Fiber Foods for Diverticulitis
Here’s a list of high-fiber foods suitable for individuals with diverticulitis:
- Fruits: Apples, pears, berries, bananas, oranges, and grapes. Choose fruits with the skin on for maximum fiber content.
- Vegetables: Broccoli, Brussels sprouts, carrots, spinach, kale, sweet potatoes, and green beans. Include a variety of colorful vegetables in your diet.
- Whole Grains: Whole-wheat bread, brown rice, oatmeal, quinoa, and barley. These grains provide complex carbohydrates and fiber, promoting digestive health.
- Legumes: Lentils, beans, chickpeas, and peas. These are excellent sources of fiber and protein, contributing to a balanced diet.
- Nuts and Seeds: Almonds, walnuts, flaxseeds, chia seeds, and sunflower seeds. These provide healthy fats and fiber, supporting overall health.
The Importance of Hydration
Staying hydrated is crucial for managing diverticulitis and promoting overall gut health. When you’re adequately hydrated, your body can effectively digest food, maintain regular bowel movements, and reduce the risk of constipation.
The Role of Water in Bowel Regularity
Water plays a vital role in keeping your digestive system functioning smoothly. When you’re well-hydrated, your stool becomes softer and easier to pass, reducing the strain on your digestive tract. This is especially important for individuals with diverticulitis, as straining during bowel movements can exacerbate symptoms and potentially lead to complications.
Daily Fluid Intake Recommendations
The amount of water you need to drink daily depends on various factors, including your activity level, climate, and overall health. However, a general guideline is to aim for 8 glasses of water per day. Other fluids, such as herbal teas, clear broth, and diluted fruit juices, can also contribute to your daily fluid intake.
Lifestyle Modifications for Diverticulitis
Beyond dietary changes, adopting healthy lifestyle habits plays a crucial role in managing diverticulitis and preventing flare-ups. Incorporating regular exercise, stress management techniques, and other positive lifestyle changes can significantly improve your overall well-being and reduce the risk of complications.
The Benefits of Regular Exercise
Regular physical activity can have a profound impact on your digestive health and overall well-being, particularly for individuals with diverticulitis. Engaging in moderate-intensity exercise, such as brisk walking, swimming, or cycling, can promote bowel regularity, strengthen your abdominal muscles, and improve blood flow to the digestive system. This can help prevent constipation, a major trigger for diverticulitis flare-ups.
Diverticulitis and Dietary Supplements

While a healthy diet is crucial for managing diverticulitis, some individuals may consider using dietary supplements to support their gut health. However, it’s essential to approach supplements with caution and consult a healthcare professional before incorporating them into your regimen.
Potential Benefits and Risks of Dietary Supplements, What diet with diverticulitis
Dietary supplements can potentially offer benefits for individuals with diverticulitis, but it’s crucial to understand the potential risks.
Some supplements may help reduce inflammation, support gut health, and promote healing. For instance, omega-3 fatty acids, found in fish oil supplements, have anti-inflammatory properties that might be beneficial. Probiotics, live microorganisms that promote a healthy gut microbiome, can also be helpful.
However, it’s essential to note that dietary supplements are not regulated by the Food and Drug Administration (FDA) in the same way as medications. This means that the quality and effectiveness of supplements can vary. Additionally, some supplements may interact with medications or have side effects.
The Role of Probiotics in Promoting Gut Health
Probiotics are live bacteria that are beneficial for the gut microbiome. They help maintain a balance of bacteria in the gut, which is essential for digestive health. A healthy gut microbiome is crucial for preventing diverticulitis and managing symptoms.
Probiotics can help reduce inflammation, improve digestion, and boost the immune system. Some studies suggest that probiotics may be effective in preventing and treating diverticulitis.
Supplements that May Be Helpful for Individuals with Diverticulitis
- Probiotics: Probiotics are live microorganisms that can help restore the balance of bacteria in the gut. Look for strains such as *Lactobacillus* and *Bifidobacterium*.
- Omega-3 Fatty Acids: These fatty acids have anti-inflammatory properties and may help reduce inflammation in the gut. Good sources include fish oil supplements, flaxseed oil, and chia seeds.
- Glutamine: This amino acid is essential for gut health and may help repair damaged intestinal lining. It is found in foods like poultry, fish, and dairy products, but supplements are also available.
- Zinc: This mineral is important for immune function and wound healing. It is found in foods like oysters, red meat, and beans, but supplements can also be helpful.
It’s important to note that these supplements are not a substitute for a healthy diet and lifestyle modifications. Always consult with a healthcare professional before taking any supplements, especially if you have underlying health conditions or are taking medications.
Seeking Professional Advice
It is crucial to remember that this information is for general knowledge and should not replace professional medical advice. While this guide provides a comprehensive overview of dietary considerations for diverticulitis, it is essential to consult with a healthcare professional for personalized recommendations.
The Importance of Personalized Dietary Guidance
A registered dietitian (RD) can provide tailored dietary guidance for individuals with diverticulitis. They can assess your specific needs, consider your medical history, and create a meal plan that aligns with your individual goals and preferences.
End of Discussion
Navigating the world of diverticulitis and diet can be a journey of self-discovery. By embracing a personalized approach that incorporates the principles Artikeld in this guide, you can empower yourself to manage your condition effectively. Remember to consult with a healthcare professional for personalized advice and to address any specific concerns you may have. With a mindful approach to diet and lifestyle, you can take control of your health and experience a more comfortable and fulfilling life.
Expert Answers
What is the difference between diverticulosis and diverticulitis?
Diverticulosis refers to the presence of pouches in the colon, while diverticulitis occurs when these pouches become inflamed or infected.
Can diverticulitis be prevented?
While there is no guaranteed way to prevent diverticulitis, a high-fiber diet and a healthy lifestyle can significantly reduce your risk.
What are some high-fiber foods I can eat?
Good sources of fiber include fruits, vegetables, whole grains, legumes, and nuts.
Is it okay to take fiber supplements for diverticulitis?
It’s best to consult with your doctor before taking fiber supplements, as they may not be appropriate for everyone.
What should I do if I experience a diverticulitis flare-up?
If you experience severe pain, fever, or other concerning symptoms, seek immediate medical attention.
A diet for diverticulitis aims to reduce inflammation and promote healing in the digestive tract. It often involves consuming foods that are high in fiber, such as fruits, vegetables, and whole grains, but avoiding foods that are difficult to digest, like seeds and nuts.
To learn more about the benefits of a high-fiber diet, you can check out this article on what is good diet food. Ultimately, a diet for diverticulitis should be tailored to your individual needs and preferences, so it’s always a good idea to consult with your doctor or a registered dietitian.
A diverticulitis diet focuses on high-fiber foods to promote regular bowel movements and prevent further inflammation. It’s important to note that managing high triglycerides, often associated with unhealthy fats and sugar intake, is crucial for overall health, and a diet rich in fruits, vegetables, and whole grains can be beneficial in this regard.
Check out this resource on how to lower triglycerides with diet to understand how to incorporate these changes effectively. This approach not only helps with diverticulitis but also contributes to a healthier lifestyle overall.
A diverticulitis diet focuses on easily digestible foods, often requiring a change in eating habits. This might involve freezing portions of meals for later consumption, but it’s important to know how long do foods last in the freezer to ensure safety and quality.
Understanding freezer storage times can help you plan meals and manage your diverticulitis diet effectively.