What type of diet for diverticulitis is a question many individuals with this condition ask. Diverticulitis, a common gastrointestinal ailment, involves small pouches forming in the colon, which can become inflamed or infected. Understanding the role of diet in managing diverticulitis is crucial for promoting healing and preventing flare-ups. A balanced dietary approach can significantly impact the severity and frequency of symptoms, empowering individuals to take control of their health.
This article delves into the complexities of diet and diverticulitis, exploring the benefits of different dietary approaches, including high-fiber and low-residue diets. We’ll examine the foods that should be included and avoided, providing practical advice for meal planning and preparing healthy meals. Furthermore, we’ll discuss the importance of staying hydrated and the potential benefits of probiotics. By understanding the nuances of diet and diverticulitis, individuals can make informed choices to support their well-being and manage this condition effectively.
Understanding Diverticulitis
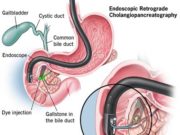
Diverticulitis is a common condition that affects the digestive system. It occurs when small, pouch-like sacs called diverticula form in the lining of the colon. These pouches can become inflamed or infected, leading to a painful condition known as diverticulitis.
Causes of Diverticulitis, What type of diet for diverticulitis
The exact cause of diverticulitis is unknown, but several factors are thought to contribute to its development. One of the primary causes is a low-fiber diet, which can lead to increased pressure in the colon and the formation of diverticula. Other factors that may play a role include:
- Age: Diverticulitis is more common in older adults, with the risk increasing after the age of 40.
- Genetics: Family history of diverticulitis can increase the risk of developing the condition.
- Obesity: Being overweight or obese can increase pressure in the colon, making diverticulitis more likely.
- Lack of Exercise: Physical inactivity can contribute to a weakened colon, increasing the risk of diverticula formation.
- Smoking: Smoking has been linked to an increased risk of diverticulitis.
Symptoms of Diverticulitis
The symptoms of diverticulitis can vary depending on the severity of the condition. Common symptoms include:
- Abdominal pain: Typically located in the lower left abdomen, the pain may be sharp, cramping, or constant.
- Fever: A high fever can indicate an infection in the diverticula.
- Nausea and vomiting: These symptoms may occur due to inflammation in the digestive tract.
- Diarrhea or constipation: Changes in bowel habits are common, with some people experiencing diarrhea, while others may have constipation.
- Blood in the stool: This symptom suggests that the diverticula may be bleeding.
Complications of Diverticulitis
While most cases of diverticulitis resolve with treatment, complications can arise in some cases. Potential complications include:
- Abscess: A collection of pus may form near the inflamed diverticula, requiring drainage.
- Peritonitis: Inflammation of the peritoneum, the lining of the abdominal cavity, can occur if the infection spreads.
- Fistula: An abnormal connection between the colon and other organs or tissues can develop.
- Obstruction: A blockage in the colon can occur if the inflamed diverticula narrow the passage.
The Role of Diet in Diverticulitis Management
Diet plays a crucial role in managing diverticulitis, a condition that affects the digestive system. By making dietary changes, individuals can help reduce inflammation, minimize pain, and prevent future flare-ups. Understanding the connection between diet and diverticulitis is essential for effective management of the condition.
Dietary Changes for Diverticulitis Management
Dietary changes are essential for managing diverticulitis. A high-fiber diet is generally recommended to promote regular bowel movements and prevent constipation, which can contribute to diverticulitis flare-ups. However, during a flare-up, it’s important to temporarily reduce fiber intake to allow the colon to rest and heal.
The High-Fiber Diet for Diverticulitis
After an acute diverticulitis episode, a high-fiber diet is often recommended to promote gut health and prevent future flare-ups. This approach aims to strengthen the digestive system and reduce the risk of diverticula forming and becoming inflamed.
Benefits of a High-Fiber Diet for Diverticulitis
A high-fiber diet can be beneficial for people with diverticulitis by promoting regular bowel movements and helping to prevent constipation. Fiber adds bulk to stool, making it easier to pass through the digestive tract. This can help to reduce pressure on the colon, which can reduce the risk of diverticula forming and becoming inflamed.
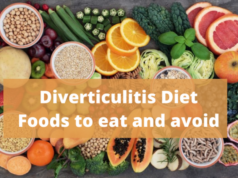
High-Fiber Foods for Diverticulitis
A balanced diet rich in fiber is crucial for managing diverticulitis. Here is a list of high-fiber foods that can be beneficial:
- Fruits: Apples, pears, berries, bananas, oranges, and grapes are good sources of fiber.
- Vegetables: Broccoli, Brussels sprouts, carrots, green beans, spinach, and sweet potatoes are excellent sources of fiber.
- Whole Grains: Brown rice, quinoa, oatmeal, whole-wheat bread, and pasta are excellent sources of fiber.
- Legumes: Beans, lentils, and peas are excellent sources of fiber and protein.
- Nuts and Seeds: Almonds, walnuts, chia seeds, flaxseeds, and sunflower seeds are good sources of fiber and healthy fats.
Gradually Increasing Fiber Intake
It’s essential to increase fiber intake gradually to avoid discomfort and potential complications. Starting with a small amount and gradually increasing it over several weeks can help your body adjust.
- Start Slowly: Begin by adding one or two servings of high-fiber foods to your daily diet.
- Listen to Your Body: Pay attention to how your body responds to the increased fiber intake. If you experience bloating, gas, or discomfort, reduce the amount of fiber you consume and gradually increase it again.
- Stay Hydrated: Drinking plenty of water is crucial when increasing fiber intake, as it helps to move fiber through the digestive system.
- Consult Your Doctor: It’s essential to talk to your doctor about how much fiber is appropriate for you. They can help you create a personalized diet plan that meets your individual needs.
The Low-Residue Diet for Diverticulitis
A low-residue diet is a temporary dietary approach used to manage acute diverticulitis flare-ups. During a flare-up, the digestive tract becomes inflamed, and consuming high-fiber foods can worsen symptoms. A low-residue diet helps reduce the amount of undigested food in the intestines, easing the pressure on the inflamed areas and promoting healing.
Foods to Include in a Low-Residue Diet
A low-residue diet focuses on easily digestible foods with low fiber content. This includes:
- Refined grains: White bread, white rice, pasta, and crackers.
- Lean protein: Chicken, fish, tofu, and eggs.
- Low-fiber fruits and vegetables: Bananas, peeled apples, ripe peaches, cooked carrots, and zucchini.
- Dairy: Milk, yogurt, and cheese.
- Broths and soups: Clear broths and soups made with low-fiber vegetables.
- Cooked, tender meats: Chicken, fish, and lean ground beef.
- Well-cooked vegetables: Cooked carrots, squash, zucchini, and peeled potatoes.
- Refined grains: White rice, white bread, and pasta.
Duration of a Low-Residue Diet
The duration of a low-residue diet depends on the severity of the diverticulitis flare-up and the individual’s response to treatment. Generally, it is recommended to follow a low-residue diet for 3-7 days during an acute flare-up. Once symptoms subside, a gradual transition to a high-fiber diet is recommended.
Foods to Avoid with Diverticulitis
While a high-fiber diet is generally recommended for preventing diverticulitis, during a flare-up, it’s crucial to avoid certain foods that can irritate the digestive system and worsen symptoms. These foods are known to increase the pressure in the colon, potentially aggravating inflammation and pain.
Foods to Avoid During a Diverticulitis Flare-Up
These foods should be avoided during a flare-up to minimize irritation and promote healing:
| Food Group | Examples |
|---|---|
| High-Fiber Foods |
|
| High-Fat Foods |
|
| Spicy Foods |
|
| Alcohol and Caffeinated Beverages |
|
| Other Irritants |
|
Other Dietary Considerations
Beyond the specific foods you eat, there are other dietary factors that can significantly impact your recovery from diverticulitis. These considerations can help you manage symptoms and promote overall gut health.
Staying Hydrated
Staying hydrated is crucial during a diverticulitis flare-up. When you are dehydrated, your body struggles to digest food effectively, which can worsen symptoms. Adequate hydration also helps to soften stools, making it easier to pass them and reducing strain on the digestive system.
- Aim to drink at least 8 glasses of water per day, especially during a flare-up.
- Other hydrating options include clear broth, herbal tea, and diluted fruit juice.
- Avoid sugary drinks, as they can dehydrate you.
The Role of Probiotics
Probiotics are live bacteria that are beneficial for your gut health. They can help to restore the balance of bacteria in your gut, which may be disrupted during a diverticulitis flare-up. Some research suggests that probiotics may help to reduce the frequency and severity of diverticulitis flares.
- Probiotics are available in supplement form or as part of fermented foods like yogurt, kefir, and sauerkraut.
- It’s essential to choose probiotic supplements that contain strains specifically shown to be beneficial for gut health.
- Consult with your doctor before taking probiotics, especially if you have any underlying health conditions.
Meal Planning and Preparation
Meal planning can be helpful in managing diverticulitis, as it allows you to prepare healthy and easy-to-digest meals that meet your dietary needs.
- Plan your meals in advance, keeping in mind your current dietary restrictions and preferences.
- Prepare meals in bulk and freeze portions for easy reheating on busy days.
- Use a slow cooker to prepare nutritious and flavorful meals without the need for excessive cooking.
Consulting a Healthcare Professional
While understanding the role of diet in managing diverticulitis is crucial, it’s essential to remember that dietary changes alone cannot cure the condition. Consulting a healthcare professional is paramount for a personalized approach to managing diverticulitis.
A doctor or registered dietitian can provide tailored recommendations based on your individual needs, medical history, and the severity of your condition. They can help you navigate the complexities of diet and diverticulitis, ensuring your dietary choices are safe and effective.
Personalized Dietary Recommendations
Diverticulitis is a complex condition, and individual needs vary significantly. What works for one person may not be suitable for another. A healthcare professional can assess your specific situation and recommend a diet plan that addresses your unique needs.
For example, someone with mild diverticulitis might benefit from a high-fiber diet, while someone with a more severe case might require a low-residue diet during the acute phase.
Potential Risks of Self-Treating
Self-treating diverticulitis with diet alone can be risky. Without proper medical guidance, you may inadvertently make dietary choices that worsen your condition or delay necessary medical interventions.
For instance, adopting a high-fiber diet without consulting a doctor could potentially exacerbate symptoms during an acute episode.
It’s crucial to remember that diet is just one aspect of managing diverticulitis. Consulting a healthcare professional is essential for a comprehensive approach that ensures your safety and well-being.
Final Summary
Navigating the world of diet and diverticulitis can be challenging, but by understanding the principles Artikeld in this article, individuals can take control of their health and manage this condition effectively. Remember to consult a healthcare professional for personalized dietary recommendations and to address any concerns. With a balanced approach, individuals can live fulfilling lives while managing their diverticulitis.
Commonly Asked Questions: What Type Of Diet For Diverticulitis
What is the best way to prevent diverticulitis flare-ups?
Maintaining a healthy diet with adequate fiber intake, managing stress, and avoiding foods that trigger flare-ups are key to preventing diverticulitis flare-ups. Regular exercise and maintaining a healthy weight can also be beneficial.
Can I eat fruits and vegetables if I have diverticulitis?
Yes, fruits and vegetables are generally beneficial for diverticulitis, especially high-fiber options. However, during acute flare-ups, you may need to avoid certain types of fruits and vegetables, such as those with seeds or skins, as they can be difficult to digest. Consult your doctor or a registered dietitian for personalized advice.
How long should I follow a low-residue diet?
The duration of a low-residue diet depends on the severity of your diverticulitis flare-up. Your doctor will advise on the appropriate length of time, typically a few days to a week, after which you can gradually transition back to a high-fiber diet.
A diverticulitis diet typically involves avoiding foods that can irritate the digestive tract, such as seeds, nuts, and popcorn. If you’re looking for a more comprehensive guide to managing your diet, you might want to check out if diet , which offers detailed information on various dietary approaches.
The goal is to find a diet that works best for you, helping you manage symptoms and promote gut health.
A diet for diverticulitis often involves high-fiber foods to promote healthy digestion. This can be tricky when breastfeeding, as your diet directly impacts your baby’s health. A balanced diet is crucial, and you can find helpful tips on the best diet when breastfeeding.
While breastfeeding, you should avoid high-fiber foods, as they can worsen diverticulitis symptoms. Consult your doctor to create a safe and effective diet plan that addresses both your needs and your baby’s.
A diverticulitis diet focuses on high-fiber foods to promote healthy digestion. It’s important to note that while diet pills might help with weight loss, they don’t address the underlying causes of diverticulitis. If you’re considering diet pills, it’s essential to consult with a doctor and understand the potential risks and benefits, such as those discussed in this article about what diet pills actually work.
Focusing on a high-fiber diet and regular exercise is often the best approach for managing diverticulitis and improving overall health.